The Reproductive Health Impact Study (RHIS) is a comprehensive research initiative that analyzed the effects of federal and state policy changes on publicly funded US family planning care from 2017 to 2024. The Guttmacher Institute worked with research and policy partners in four states—Arizona, Iowa, New Jersey and Wisconsin—to document the impact of these policies on family planning service delivery and the patients who rely on this care.
New Jersey was selected as an RHIS focus state in 2019 because of its long-established family planning network and policies that are generally supportive of sexual and reproductive health. This supportive environment was anticipated to provide a protective buffer against federal policy attacks, compared with the environments in states that are less supportive of sexual and reproductive health.
The information in this state profile reflects the landscape in New Jersey during the RHIS study period. For the most current information about the sexual and reproductive health research and policy landscape in New Jersey, visit our state information page.
Overall Findings
The RHIS findings demonstrate that restrictions on sexual and reproductive health and rights undermine people’s reproductive autonomy through negative outcomes at the patient, provider and system levels. Additional and unexpected disruptions to the landscape during the study period, such as the COVID-19 pandemic and the US Supreme Court’s Dobbs v. Jackson Women’s Health Organization decision overturning Roe v. Wade, exacerbated the harms of restrictive policies.
The main study findings include:
- All types of sexual and reproductive health care are inextricably linked, and policy restrictions on sexual and reproductive health care have broader implications.
- Programs and policies that support person-centered care and focus on sexual and reproductive health equity are key to ensuring reproductive autonomy for all patients.
- Cost is a significant barrier to patients’ ability to access care and achieve reproductive autonomy.
- Person-centered contraceptive care is essential because contraceptive preferences vary.
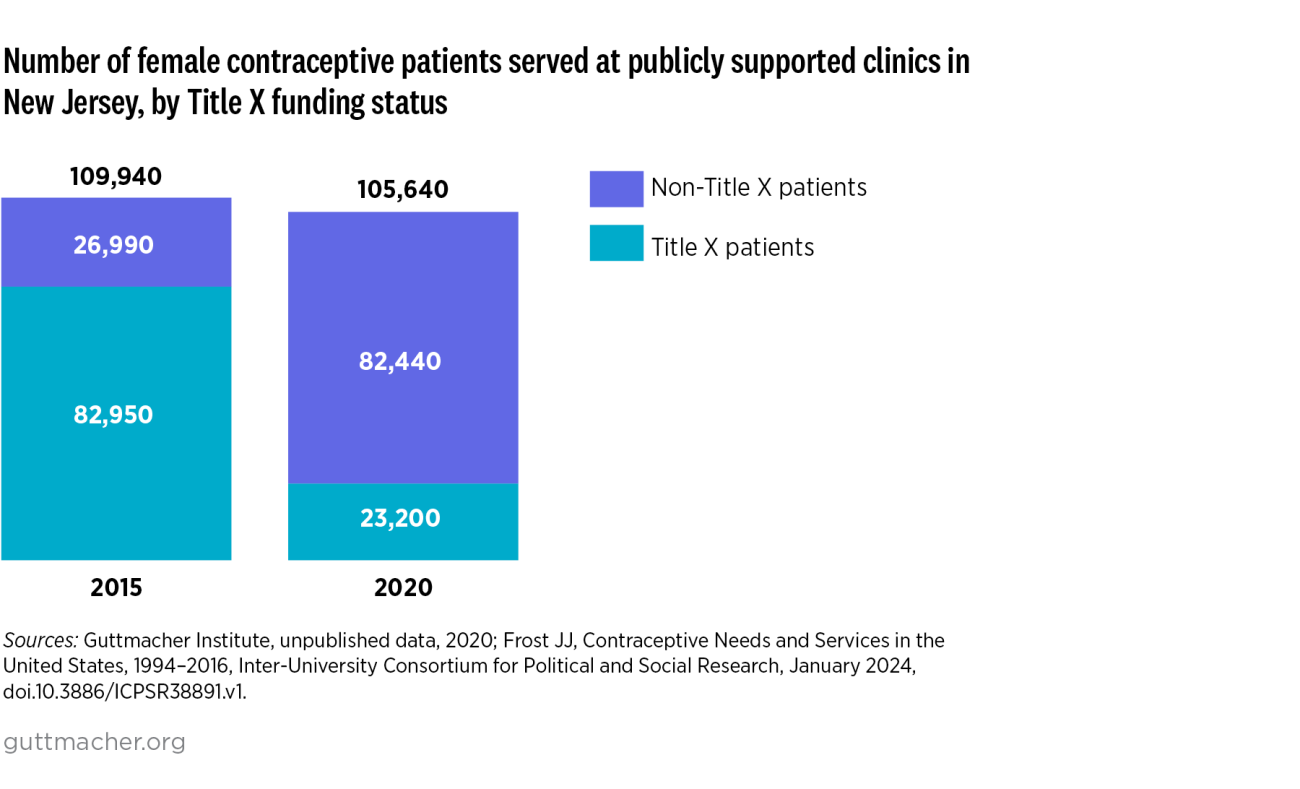
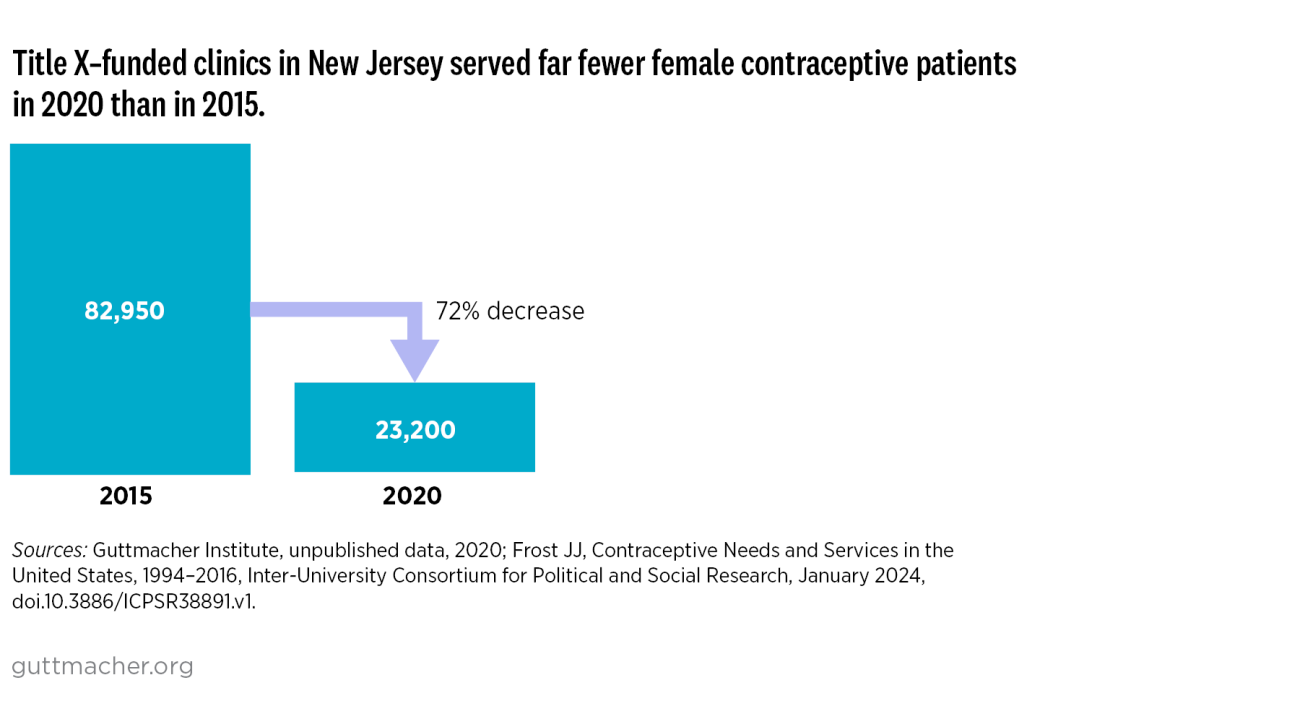
- Publicly funded family planning programs, including Title X, are critical to making contraceptive services affordable.
New Jersey’s Sexual and Reproductive Health Landscape, 2017–2024
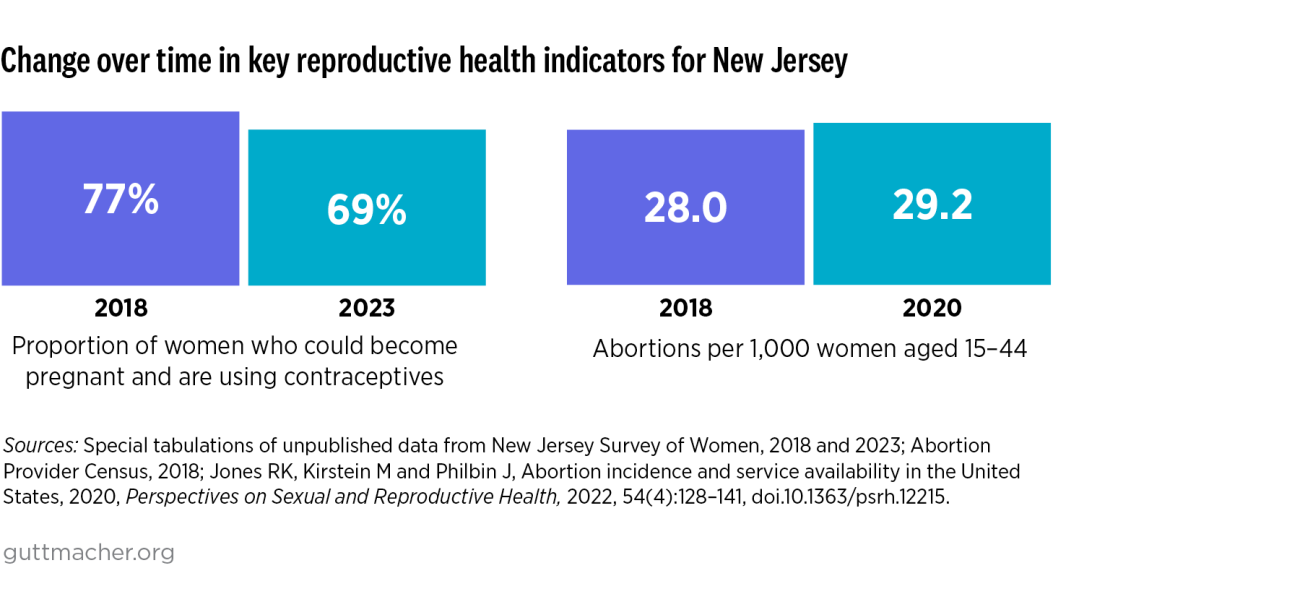
In 2020, New Jersey was home to 2 million women of reproductive age (15–49), 23% of whom had incomes below 200% of the federal poverty level.1 In the same year, about 411,200 women in New Jersey were considered likely to have a need for publicly supported contraceptive care.2 Additionally, 10.8% of women in New Jersey aged 15–49 were uninsured in 2019, compared with a national average of 12%.