Corrected December 6, 2017. See note below.
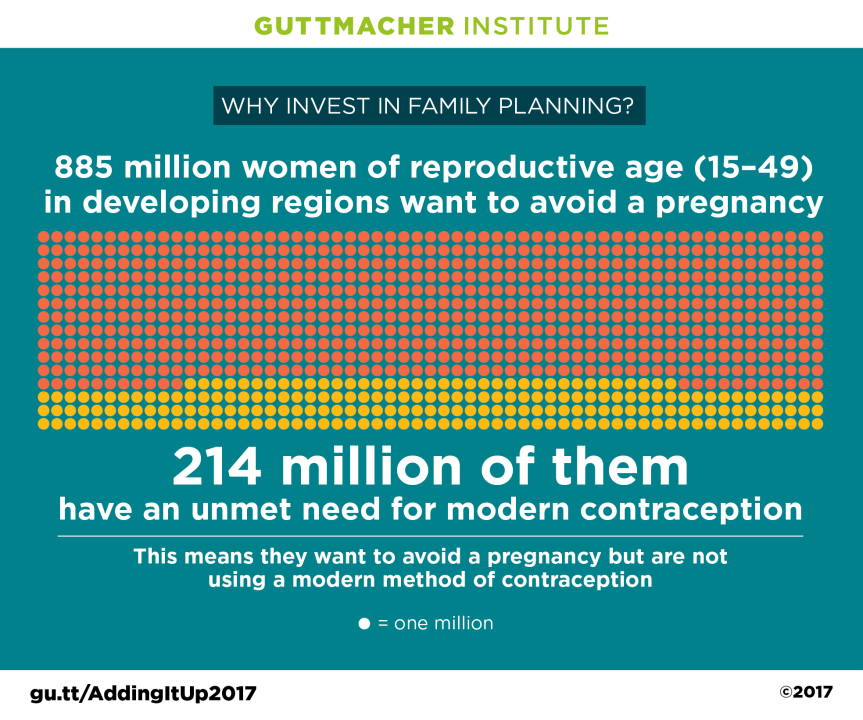
A new study published today by the Guttmacher Institute finds that contraceptive services and maternal and newborn health (MNH) services fall far short of needs in developing regions. The study, Adding It Up: Investing in Contraception and Maternal and Newborn Health, 2017, finds that 214 million women in developing countries want to avoid pregnancy but—for a variety of reasons—are not using a modern method of contraception. In addition, tens of millions of women do not receive the basic pregnancy and delivery care they need to protect their health and that of their newborns: An estimated 47 million women giving birth this year will receive fewer than four antenatal care visits, and 35 million women giving birth will not deliver in a health facility.
Though progress has been slow, there has been a steady increase in the use of modern contraceptive methods in developing countries, even as the number of women of reproductive age has grown. As a result, the number of women with an unmet need for contraception has declined over the past three years, from 225 million in 2014. However, ongoing investments in family planning are essential to maintain these gains and make further progress. Ensuring that women with an unmet need for modern contraception overcome barriers to effective contraceptive use is crucial, since they account for 84% of all unintended pregnancies in developing regions.
"Meeting the need for family planning and pregnancy-related health care in developing regions will have a dramatic impact on the lives of millions of women and their families," says Ann Starrs, President and CEO of the Guttmacher Institute. "Far too many women and newborns still lack access to these essential services."
The study also finds that among women giving birth in developing regions in 2017, only 63% receive four or more antenatal care visits and 72% deliver in a health facility. Wide disparities exist across regions. For example, these proportions are lowest in Africa, where only half of pregnant women receive four or more antenatal visits and just over half give birth in a health facility. By contrast, in Latin America and the Caribbean, close to nine in 10 women receive four or more antenatal visits, and more than nine in 10 women give birth in a facility.
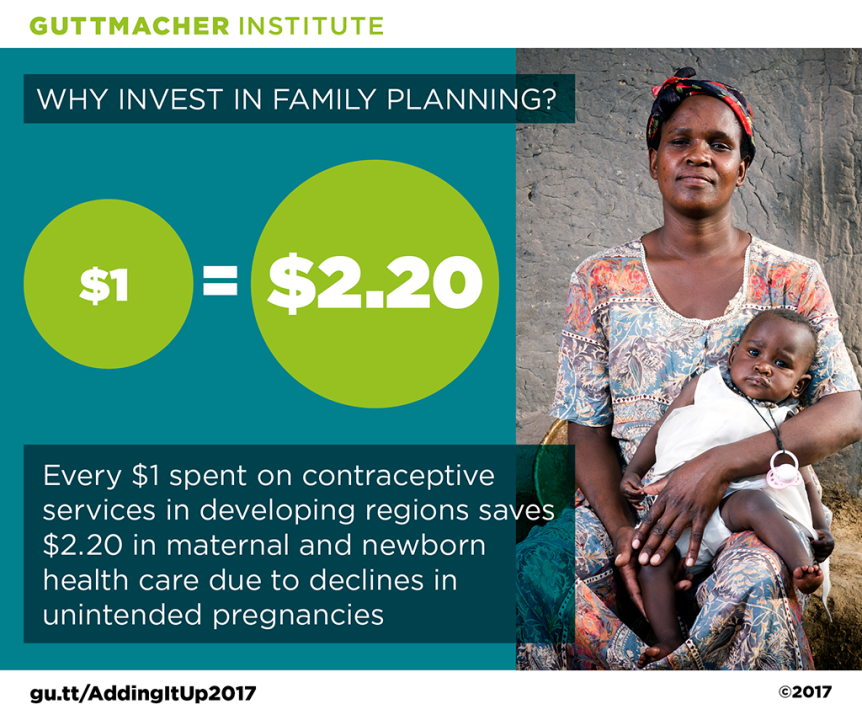
Fully meeting contraceptive and MNH care needs in developing regions can be achieved by spending $53.6 billion annually, or just $8.56 per person per year (in 2017 U.S. dollars). The new research shows that meeting the needs for modern contraception and pregnancy-related care together is a cost-saving investment. Investments in contraceptive services substantially lower the cost of MNH care by decreasing the incidence of unintended pregnancies. As a result, for each additional dollar spent on contraceptive services above the current level, the cost of pregnancy-related care is reduced by $2.20.
"Investing in both contraceptive care and essential maternal and newborn care has the greatest impact on preventing needless deaths of women and newborns," says Dr. Jacqueline E. Darroch, senior fellow at the Guttmacher Institute and lead author of the study. "Maternal deaths would drop to a quarter of current levels and newborn deaths would drop to less than one-fifth of current levels with an investment of just $8.56 per person per year."
The impact of this increased investment would be dramatic and wide-ranging. Meeting the need for modern contraception in developing regions and ensuring that pregnant women and their newborns receive essential care would result in the following declines from current 2017 levels:
- 67 million fewer unintended pregnancies (a 75% decline)
- 23 million fewer unplanned births (a 76% decline)
- 36 million fewer induced abortions (a 74% decline)
- 2.2 million fewer newborn deaths (an 80% decline)
- 224,000 fewer maternal deaths (a 73% decline)
Beyond this, investing in these services will result in broad social and economic benefits for women, their partners and families, and for societies as a whole. These benefits include increases in women’s and children’s education, increases in women’s earnings and reductions in poverty.
Reducing barriers to the provision of accessible, acceptable sexual and reproductive health care will require addressing policy restrictions, poor-quality services, and social and economic factors that prevent people from obtaining or using needed services. Moreover, previous research has shown that women give a range of reasons for not using modern contraceptive methods, such as concerns about side effects and health risks, and the belief that they are not at risk of getting pregnant because of infrequent sex. This points to an urgent need for high-quality contraceptive services that offer a wide range of methods and include accurate, comprehensive counseling.
"Meeting the sexual and reproductive health needs of women in developing regions is an achievable and affordable goal if world leaders give this global health priority the urgent attention it needs," says Starrs.
This study was made possible by UK Aid from the UK Government and grants from the Bill & Melinda Gates Foundation and the John D. and Catherine T. MacArthur Foundation. The views expressed are those of the authors and do not necessarily reflect the positions and policies of the donors.
Note: Changes were made to correct errors in the coverage of contraceptive and maternal health services and the calculation of cost estimates in Adding It Up: Investing in Contraception and Maternal and Newborn Health, 2017. None of these corrections change the study’s summary findings or conclusions. For details, see the errata at the end of the online supplementary tables (addingitup2017-supplementary-tables.xlsx) at https://www.guttmacher.org/fact-sheet/adding-it-up-contraception-mnh-2017.
For more information, see the full fact sheet:
Adding It Up: Investing in Contraception and Maternal and Newborn Health, 2017, by Jacqueline E. Darroch et al. (en español) (en français)