This report examines trends in sexual behavior and contraceptive use among high school students in the United States from 2013 to 2017, including differences by gender, grade and race and ethnicity. The data analyzed for this report are from the 2013, 2015 and 2017 Youth Risk Behavior Survey, conducted by the Centers for Disease Control and Prevention.
Sexual Behavior and Contraceptive and Condom Use Among U.S. High School Students, 2013‒2017

Author(s)
Elizabeth Witwer, Rachel K. Jones and Laura D. LindbergReproductive rights are under attack. Will you help us fight back with facts?
Key Points
- Ensuring that adolescents have access to the information and services they need to lead healthy sexual lives is essential to their sexual and reproductive health, rights and well-being. Young people must have the appropriate resources and tools to determine if and when they want to have a child and to prevent HIV and other sexually transmitted infections (STIs).
- To provide insight into the sexual health and contraceptive use of U.S. high school students, this report analyzes data from the 2013, 2015 and 2017 rounds of the nationally representative Youth Risk Behavior Survey, conducted by the Centers for Disease Control and Prevention.
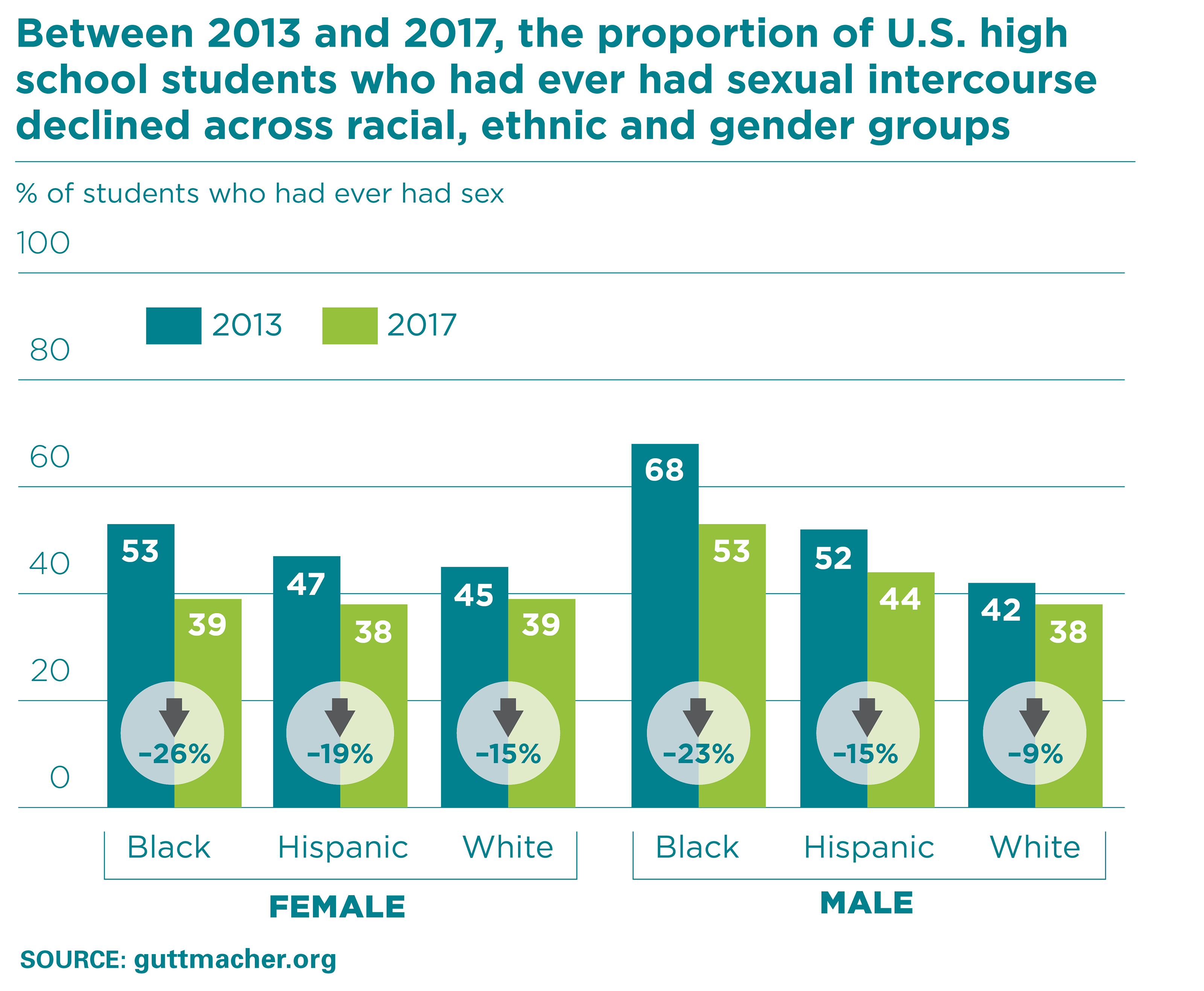
- Over the past five years, significant changes in students’ sexual and contraceptive behaviors were found, including a decrease between 2013 and 2017 in the proportion of students who had ever had sexual intercourse.
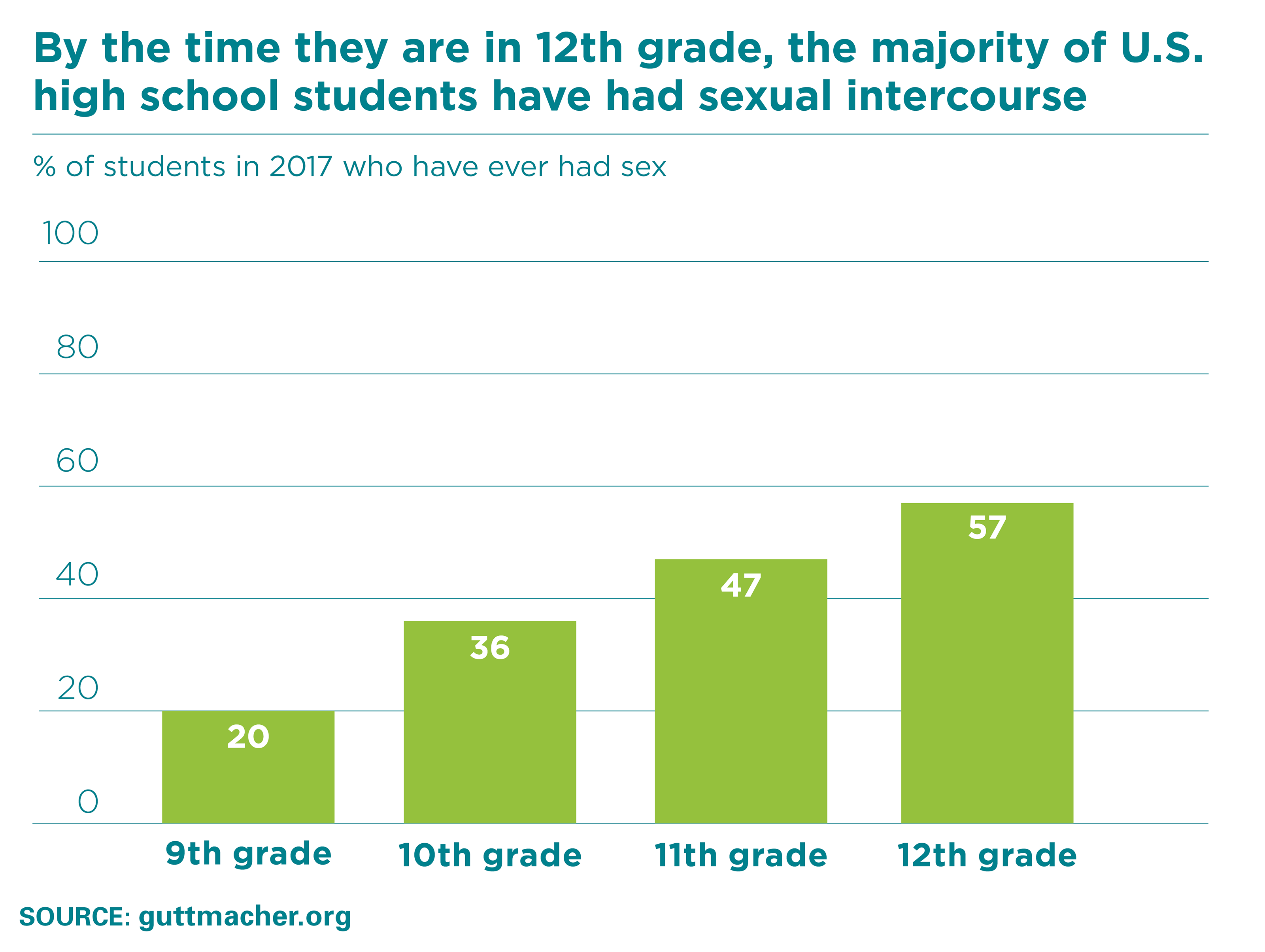
- Adolescence is a time of development and transition, and young people are more likely to begin having sex as they grow older. In 2017, more than half of 12th-graders had had sex, while one-fifth of ninth-graders had done so.
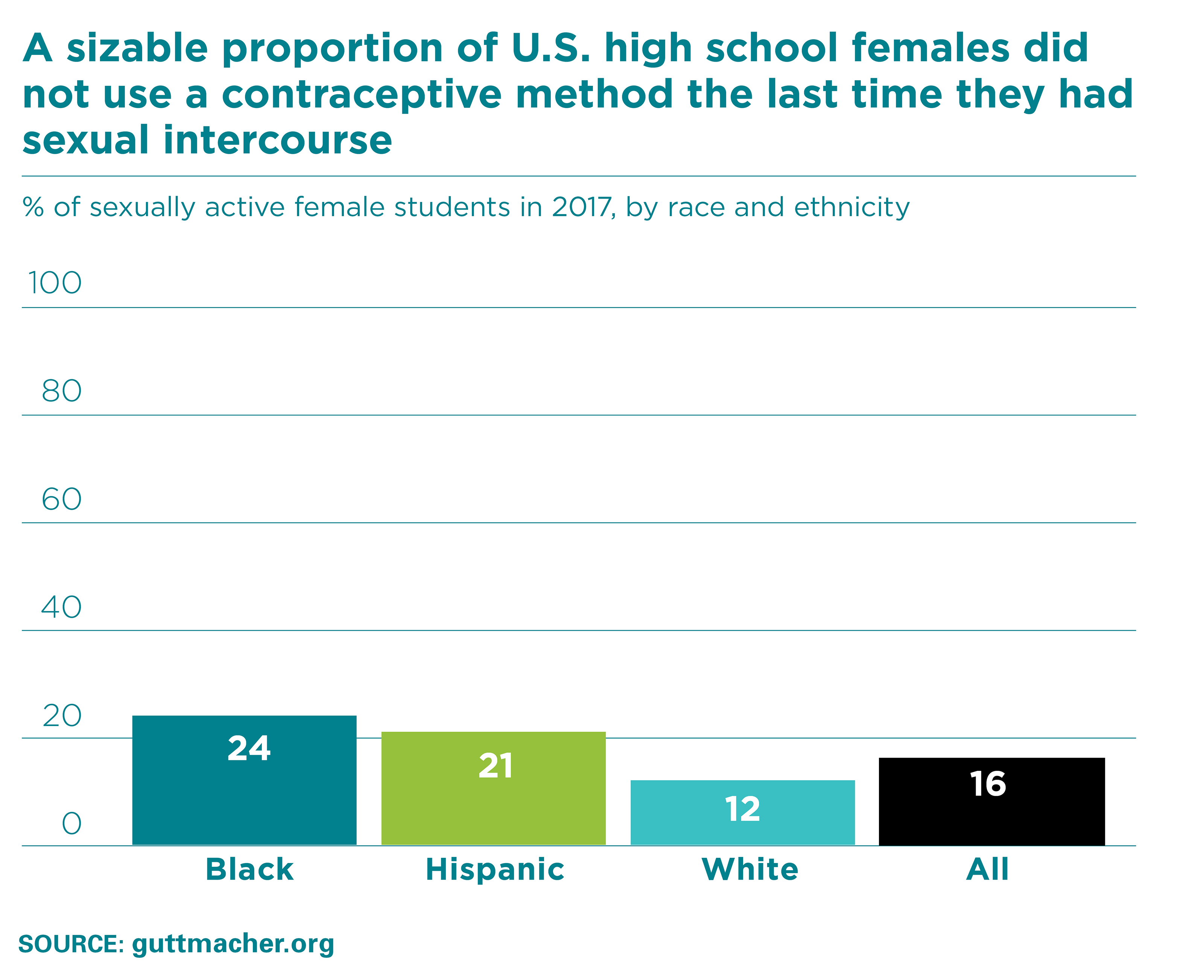
- As reported in the 2017 survey, most students used a contraceptive method the last time they had sexual intercourse, but more than one in 10 did not. Among the youngest high school students, one in five did not use a method, and this proportion has not changed since 2013.
- While there was no shift in female students’ overall contraceptive use between 2013 and 2017, there was a significant increase in the use of IUDs and implants (from 2% to 5%).
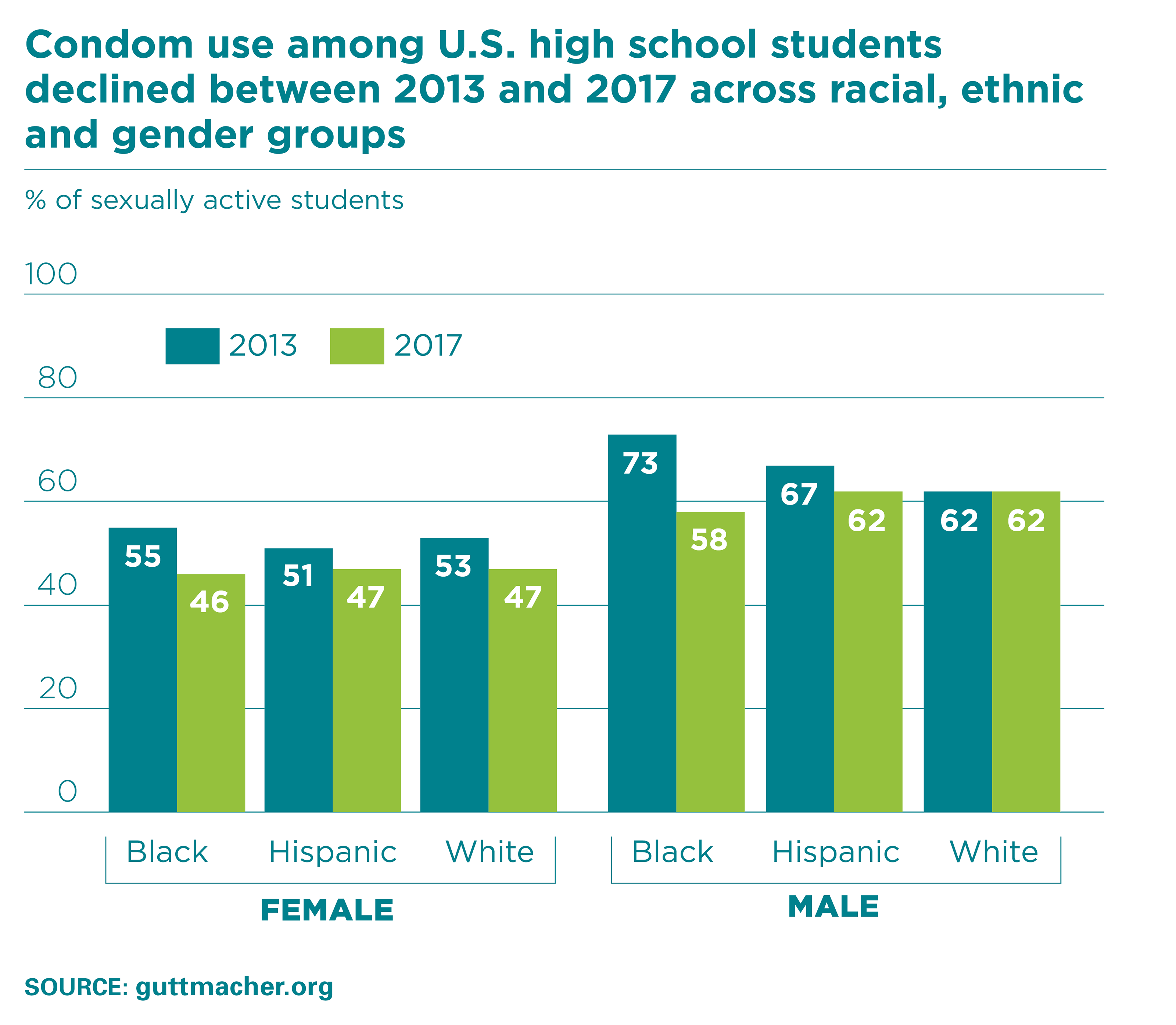
- The majority of sexually active high school students—54% in 2017—used a condom at their last sexual intercourse, but such use has declined since 2013.
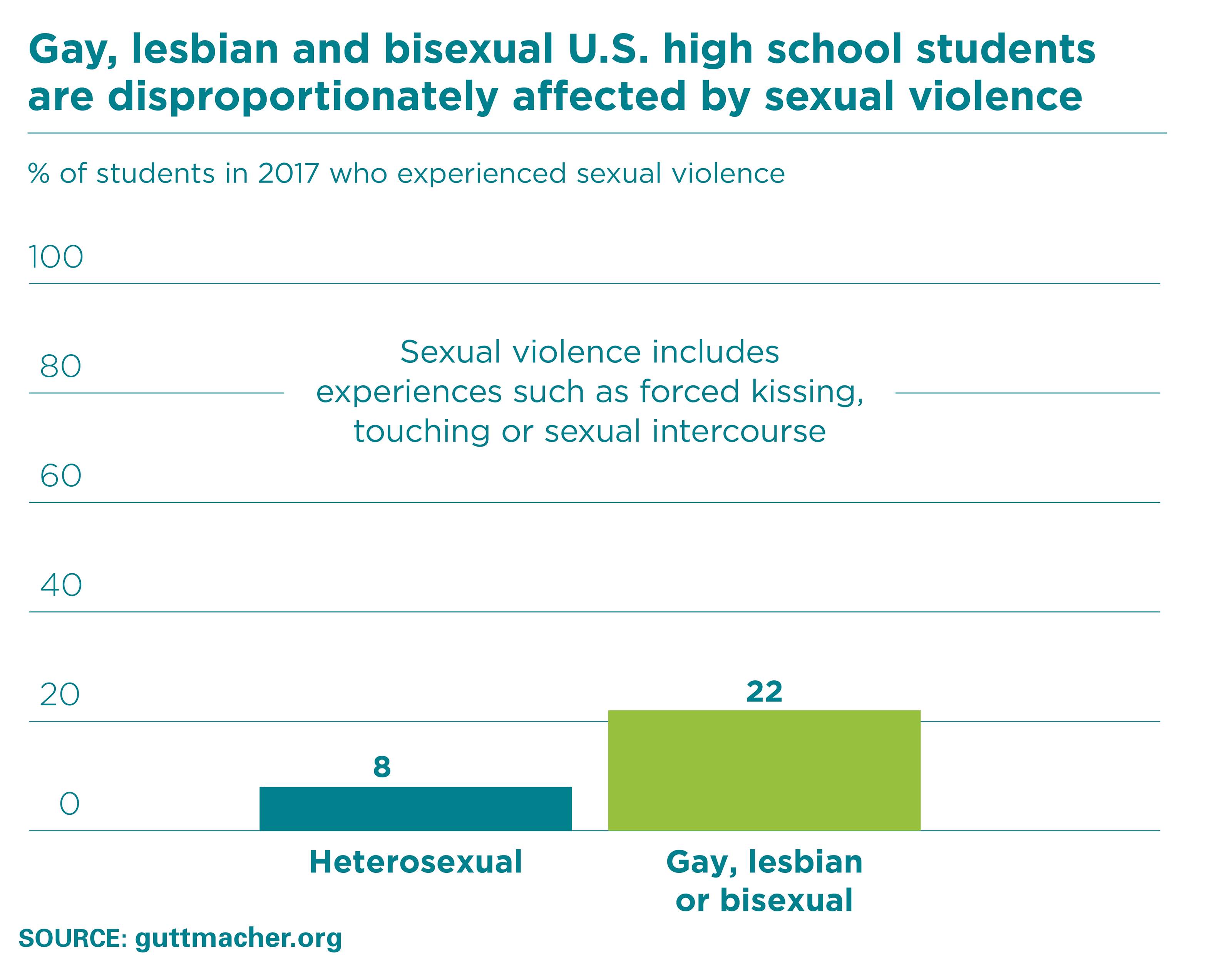
- In 2017, one of every 10 students reported experiencing sexual violence, such as forced kissing, touching or sexual intercourse, in the past year; this was more common among females (15%) than males (4%). Students who identified as gay, lesbian or bisexual were substantially more likely to report sexual violence in the past year (22%) than were heterosexual students (8%), and this disparity was found among both males and females.
- Evidence indicates that while young people often make contraceptive and behavioral decisions that help prevent unintended pregnancy, HIV infection and other STIs, there is a need for increased efforts to provide them with comprehensive sex education and access to sexual health services, including contraception.
Introduction
This report examines recent patterns in sexual activity and contraceptive use among U.S. high school students. We analyzed data from the 2013, 2015 and 2017 rounds of the Youth Risk Behavior Survey (YRBS), a national survey conducted by the Centers for Disease Control and Prevention (CDC). We focused on sexual activity and contraceptive use because these measures are the main drivers of two frequently monitored public health outcomes in the lives of young people: sexually transmitted infections (STIs), including HIV, and adolescent pregnancy. While the CDC publishes biannual reports on national survey data, as well as long-term trends assessments on health behaviors,1,2 the present report examines patterns in sexual and reproductive health behaviors between 2013 and 2017 to highlight changes that may inform recent trends in adolescent pregnancy and STI rates.
The adolescent pregnancy rate (which includes births, abortions and miscarriages) among 15‒19-year-olds has been declining for several decades, but this decrease has accelerated over the last decade. For example, the pregnancy rate among this age-group dropped 38% between 2006 and 2013 (from 71 to 43 pregnancies per 1,000 women).3 The adolescent birthrate declined by more than 45% between 2000 and 2014, while the abortion rate for this group fell by more than half over this period.3 Ongoing research has indicated that improvements in contraceptive use were a primary driving factor behind these trends.4,5 However, three-fourths of pregnancies among adolescents are reported to be unintended, and one-fourth end in abortion.3 This suggests that many young people who become pregnant would have preferred to avoid pregnancy or to have delayed childbearing until a later time. This report provides recent trend information on sexual activity and contraceptive use among high school students in an effort to help understand if we can expect these trends to continue.
In contrast to adolescent pregnancy rates, the rates of STIs—including chlamydia, gonorrhea and syphilis—have been rising for some groups of adolescents in recent years. For example, the prevalence of chlamydia among 15‒24-year-old males increased 14% between 2012 and 2016, and that of syphilis increased by more than 50% among both males and females in this age-group over this time period.6 Black 15‒19-year-olds experience substantially higher rates of all three STIs relative to their white counterparts.7 Furthermore, among all individuals with HIV in 2016, one in five were aged 13‒24, and young males who have sex with males—especially those who are black or Hispanic—are disproportionately affected.8 While structural inequalities within health care and economic systems, which are not measured in the YRBS, influence differences among racial and ethnic groups, the YRBS data allow us to examine key sexual behaviors that may play a role in both the increase in STIs and subgroup differences.
Methodology
The YRBS is a nationally representative, school-based survey of U.S. high school students. This report focuses on the years 2013, 2015 and 2017 to examine recent trends in sexual behavior and contraceptive use, and uses data from 43,972 students across the three survey rounds (Table 1).
The survey includes a number of questions related to sexual behavior and contraceptive use. It asks, "Have you ever had sexual intercourse?" (Intercourse is not defined in the survey.) Information on contraceptive behavior is reported by individuals who are "sexually active," defined as having had intercourse in the past three months.
Because the YRBS collects a limited amount of demographic data, behaviors can be examined against only a few characteristics: grade, gender, race and ethnicity, and in some cases, sexual identity. The present report reflects the race and ethnicity categories used by the YRBS—Hispanic, black and white (the last two being non-Hispanic)—and excludes other racial or ethnic categories because of small sample sizes. Findings on condom use and method nonuse rely on data from both males and females, while those on use of other contraceptives are estimated from reports of female respondents only.
For all behavior outcomes, we tested for differences across survey years, and when relevant, across demographic categories within 2017. Unless stated otherwise, we focused on results that were statistically significant at p<.05. More information regarding the data, survey methodology and analysis is available in the report’s appendix and in the YRBS methods documentation.9-11
Findings
Sexual Behavior
Sexual activity is a normal part of development for many young people. The examination of recent trends in adolescents’ sexual activity can help us to better understand their experiences and associated health outcomes, as well as the kinds of information, resources and support they need to have healthy lives regardless of whether they have started having sex.
Trends in sexual behavior
- There has been a long-term decline in the proportion of high school students who have ever had sexual intercourse. In 2017, the share of students who had ever had intercourse—40%—was the lowest since 1991, when the YRBS was initiated.
- Much of the decline occurred between 1991 and 2001, followed by a stabilization until 2013.
- A statistically significant drop in the proportion of students who had ever had intercourse occurred between 2013 (47%) and 2015 (41%); the proportion remained steady to 2017 (40%).
- Male and female high school students of all racial and ethnic backgrounds were less likely to report ever having had intercourse in 2017 than in 2013; the declines were greatest among black students (Table 2).
Differences among students in 2017
- In 2017, significant differences in the share of students who had ever had intercourse were seen by gender, race or ethnicity.
- Overall, a greater proportion of male students than female students had ever had sex (41% compared with 38%).
- Eighty-five percent of high school students identified themselves as heterosexual; 2% identified as gay or lesbian and 8% as bisexual, and 4% were unsure.* Among females, 50% of individuals who identified as gay, lesbian or bisexual had had sexual intercourse, whereas 36% of those who were heterosexual had done so. Among males, there were no differences in reports of sexual intercourse by sexual identity.
- Among males, black (53%) and Hispanic (44%) students were more likely to have had intercourse than white (38%) students. There were no significant differences by race or ethnicity among female students (38–39% among all groups).
- Unsurprisingly, as students get older, they are more likely to have sex. In 2017, some 57% of 12th-graders had ever had intercourse, compared with 20% of ninth-graders. Among students who have not had sex, about one in five will start having sexual intercourse each year.
Contraceptive and Condom Use
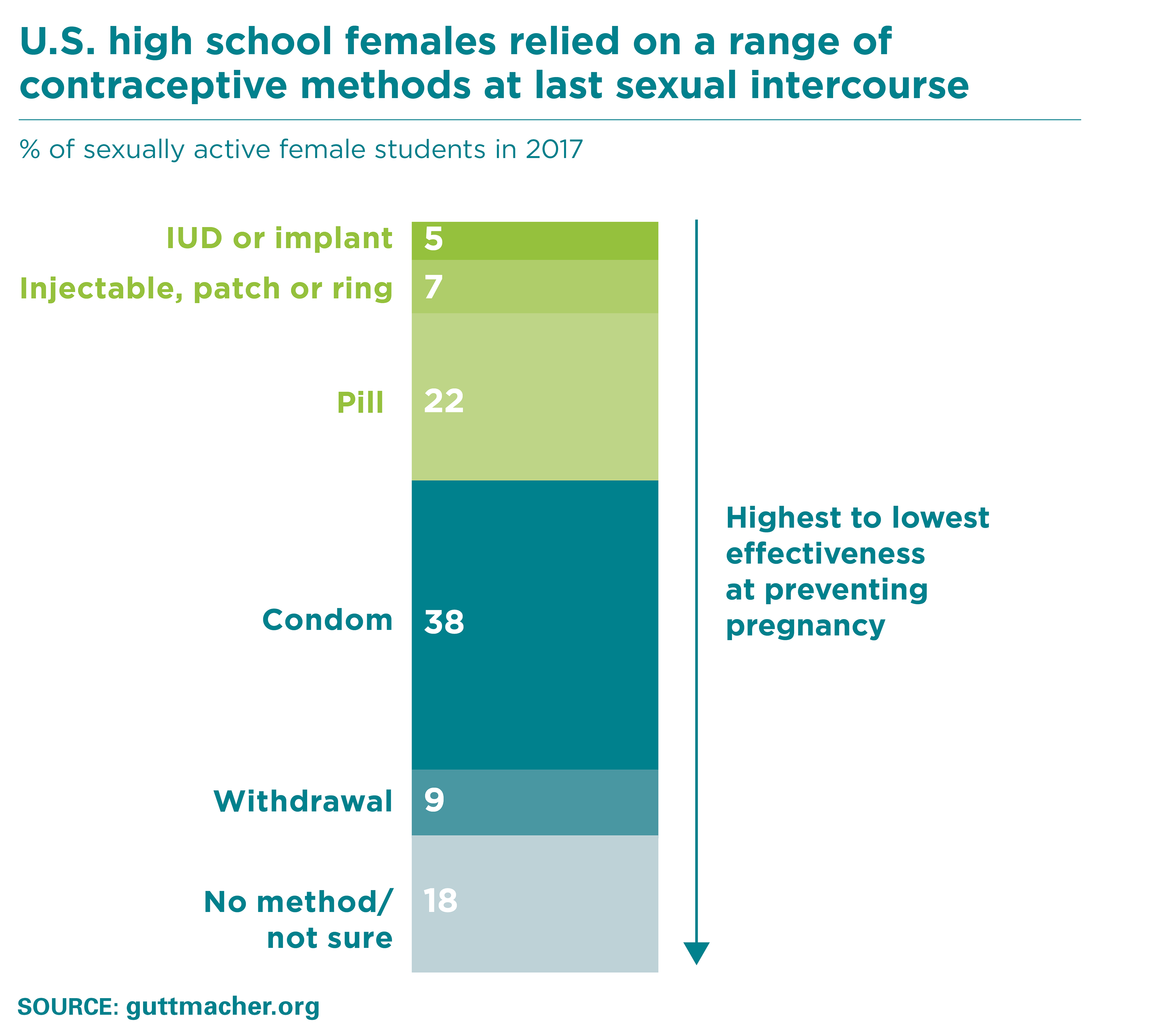
Among high school students who had had sexual intercourse in the last three months, the YRBS assessed which contraceptive methods, if any, had been used at last intercourse. We examined several categories of methods. Short-term hormonal methods, such as the pill, the patch, the injectable and the ring, are 91‒94% effective at preventing pregnancy. Long-acting reversible contraceptive (LARC) methods—the IUD and the implant—have even higher efficacy rates (greater than 99%), in part because their use is less prone to user error. Condoms, which can be used alone or at the same time as another method, are about 82% effective at reducing the likelihood of pregnancy, HIV and other STIs.12
Contraceptive use and nonuse
- Most sexually active high school students use contraceptives. In 2017, some 16% of sexually active females and 10% of males reported that they or their partner had not used any method to prevent pregnancy at last intercourse (Table 3). This level of nonuse has been unchanged since 2013.
- Contraceptive use varies by racial and ethnic background. In 2017, among sexually active females, 24% of black, 21% of Hispanic and 12% of white students reported having used no method at last sex. Among their male counterparts, 10% of black, 15% of Hispanic and 7% of white students reported that they or their partner had not used a method the last time they had intercourse.
- Older students were more likely to report that they had used a contraceptive method at last intercourse. Among those who were sexually active, nonuse was significantly higher among ninth-graders (19%) than among 11th- and 12th-graders (11% and 12%, respectively).
Prescription method use
- In 2017, some 35% of sexually active female students reported using a prescription method—IUD, implant, injectable, patch, ring or pill—the last time they had intercourse; this proportion has been largely stable since 2013 (Table 4).
- There was a significant increase in prescription method use among the oldest students; between 2015 and 2017, the proportion of females in 12th grade who reported using a prescription method at last intercourse rose from 36% to 45%.
- Among females, the prevalence of IUD or implant use more than doubled between 2013 and 2017, from 2% to 5%; most of this increase occurred in the first two years.
Differences among students in 2017
- In 2017, use of prescription contraceptives at last intercourse varied across racial and ethnic groups. Among sexually active females, 44% of white students used such a method, as did 24% of black and 20% of Hispanic students (Table 5).
- In the same year, ninth-grade females were less likely than 11th- and 12th-graders to have used a prescription method at last sex.
Condom use
- Over the five-year time period, there was a gradual decline in condom use at last intercourse among high school students, from 59% in 2013 to 54% in 2017 (Table 6). Declines were reported by both male (66% to 61%) and female (53% to 47%) students.
- When examined by both gender and race or ethnicity, the decline in condom use at last sex from 2013 to 2017 was most pronounced among black males, falling from 73% to 58%. Condom use also declined significantly among white females, from 56% in 2015 to 47% in 2017.
- While there were some differences in condom use by race and ethnicity in 2013, by 2017 the prevalence of such use was similar among all students (52‒55%).
- In 2017, some 9% of high school students used condoms and a prescription method at last intercourse (Table 7). This represented a slight but significant decrease from 2015, when 12% reported such dual method use.
Sexual Violence
All individuals have the right to decide if and when to engage in sexual activity. For some young people, sexual contact is forced or coerced. The YRBS asks students about experiences of sexual violence, such as forced kissing, touching or sexual intercourse, in the past 12 months.
Sexual violence in the past year
- In 2017, one of 10 high school students reported experiencing sexual violence in the past 12 months; this was more common among females (15%) than males (4%—Table 8).
- The proportions of black, Hispanic and white females who experienced sexual violence in the last year ranged from 11% to 17%, while those for males ranged from 4% to 6%.
- Students who identified as gay, lesbian or bisexual were substantially more likely to report sexual violence in the past year (22%) than were heterosexual students (8%), and this disparity was found among both males and females.
Discussion
The recent decline in the proportion of high school students who have ever had sexual intercourse marks an important shift following more than a decade of stability. The drivers of this decline—which was concentrated between 2013 and 2015—have not been established, and continued surveillance of trends in sexual behavior remains important. Monitoring the experiences of new cohorts of students, as well as following current students as they age, will help in understanding the transition to sexual activity among young people today.
The decrease in condom use between 2013 and 2017 raises significant public health concerns. Further research is needed to determine whether adolescents’ increased reliance on LARC methods over this period contributed to this drop, or if the emergence of biomedical HIV-prevention approaches, such as pre-exposure prophylaxis, may have played a role. Given the challenge of historically high and increasing STI rates, a better understanding of contraceptive dynamics is particularly urgent.
Notably, while our study found shifts in the types of contraceptives young people are using, the proportion of sexually active high school students who had had unprotected sex did not change over the study period. More than one in 10 did not use a method the last time they had intercourse, and these proportions were highest among black and Hispanic females. Furthermore, younger students need more support in accessing and using contraceptives, as one in five ninth-graders did not use any method of pregnancy or STI prevention the last time they had sex.
The recent inclusion of questions regarding sexual identity in the YRBS allows for enhanced understanding of young people’s sexuality. In 2017, one of 10 high school students identified as gay, lesbian or bisexual. Female students who so identified themselves were more likely than their heterosexual counterparts to have ever had intercourse, and a growing body of research is highlighting greater rates of unintended pregnancy among young lesbian and bisexual women.13 Moreover, other findings from the 2017 YRBS underscore that lesbian, gay and bisexual students are at increased risk for a number of negative outcomes, such as substance abuse, bullying, physical and sexual abuse, and suicide.1 There is a critical need for comprehensive sexuality education that is inclusive of different sexual identities, behaviors and experiences,14 and for progress in establishing a supportive and respectful environment for all young people, regardless of sexual identity or behaviors.
Finally, the prevalence of sexual violence among high school students is alarming. While female students were more likely than males to report having experienced sexual violence in the past year—about one in six—male students also experienced such violence. Such rates were even higher among gay, lesbian and bisexual students, highlighting their vulnerability to sexual violence. Students—and all young people—deserve access to unbiased health care services so they can protect themselves from HIV and other STIs. They also require access to a full range of contraceptive methods to ensure they are able to choose and use the methods that best meet their needs. Young people also need comprehensive sexual education that is unbiased and medically accurate, and that covers sexual consent to help them achieve healthy sexual relationships and lives. Policies and programs that support young people’s sexual and reproductive health are essential to ensure they have the resources and education they need to thrive.
Appendix: Methodology and Limitations
Methodology
We conducted analyses using the 2017 Youth Risk Behavior Survey combined national dataset, publicly available from the CDC. Data are gathered via paper and pencil surveys administered to public and private high school students. The YRBS has been collecting information from high school students biannually since 1991, but this report focuses on the years 2013, 2015 and 2017 in order to address recent trends in sexual behavior and contraceptive use. Method use data from 2013 on are not fully comparable with data from earlier surveys; in particular, the measurement of IUD and implant use changed beginning with the 2013 survey.
Our analytical dataset consisted of information from 43,972 respondents. All demographic variables had missing values, ranging from less than 1% for age, gender and grade to 9‒11% for measures related to sexual activity and contraceptive use. Missing cases were excluded from relevant analyses. To account for the complexity of the sampling design, we applied weights using syntax provided by the CDC.11 While the CDC tests for changes across years using linear and quadratic terms, for all outcomes, we employed unadjusted logistic regression analysis to test for differences between pairs of survey years, and for 2017, across demographic categories. In the text we report only findings that were statistically significant at p<.05. Data analyses were conducted using Stata version 15.1.
While our analysis primarily utilized the variables provided by the CDC, in a few instances we recoded or created new variables. If respondents answered yes to using a condom at last sexual intercourse in a survey question about only condom use, and in a separate question about all contraceptive methods answered that they were not sure or used withdrawal or no method at last intercourse, we recoded those individuals as having used condoms as the most effective method. Therefore, compared with CDC reporting, our report reflects slightly lower proportions of respondents reporting withdrawal, no method or uncertainty about the method used at last sex, and slightly higher prevalence of condom use as the most effective method.
Limitations
This analysis has several limitations. Most notably, the YRBS gathers information only from adolescents attending high school. Those who were not in school or who dropped out may have different sexual and contraceptive-use experiences, making generalizability of these findings to the overall population of young people inappropriate. The method used at last intercourse is the primary contraceptive measure examined in the YRBS, but consistency of use is also important. Similarly, the YRBS does not capture the use of prescription methods among adolescent females who were not currently sexually active, and thus undercounts overall use. Furthermore, some sexually active students who were not using contraceptives may have been actively or passively seeking to become pregnant, and the YRBS does not collect information on pregnancy intention.
The YRBS is not designed to examine directly the extent to which racial or ethnic differences in use of prescription contraceptives may be driven by differential access to sexual and reproductive health care, preferences for method types or other factors, such as relationship types and partner influences.15 Research on the experiences of adolescents and adults has found that differences in effective contraceptive use between white women and black or Hispanic women are greatest during adolescence,16 indicating that young women of color face unique challenges in accessing and using contraception. Moreover, YRBS data on Asian, American Indian, Alaskan Native, Hawaiian Island and multiracial students merit further examination. While analysis of single YRBS rounds may be limited by small sample sizes, analyses that pool data across years could advance understanding of the sexual health and contraceptive experiences of students among different racial and ethnic groups.
Footnotes
*Percentages do not add to 100 because of rounding.
References
1. Kann L et al., Youth Risk Behavior Surveillance—United States, 2017, Morbidity and Mortality Weekly Report, Vol. 67, No. SS-8.
2. Centers for Disease Control and Prevention (CDC), National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Youth Risk Behavior Survey: Data Summary & Trends Report, 2007–2017, no date, https://www.cdc.gov/healthyyouth/data/yrbs/pdf/trendsreport.pdf.
3. Kost K, Maddow-Zimet I and Arpaia A, Pregnancies, Births and Abortions Among Adolescents and Young Women in the United States, 2013: National and State Trends by Age, Race and Ethnicity, New York: Guttmacher Institute, 2017, https://www.guttmacher.org/report/us-adolescent-pregnancy-trends-2013.
4. Lindberg L, Santelli J and Desai S, Understanding the decline in adolescent fertility in the United States, 2007–2012, Journal of Adolescent Health, 2016, 59(5):577–583, doi:10.1016/j.jadohealth.2016.06.024.
5. Lindberg L, Santelli J and Desai S, Changing patterns of contraceptive use and the decline in rates of pregnancy and birth among U.S. adolescents, 2007–2014, Journal of Adolescent Health, 2018, 63(2):253–256, doi:10.1016/j.jadohealth.2018.05.017.
6. CDC, STDs in adolescents and young adults, 2016 Sexually Transmitted Diseases Surveillance, 2017, https://www.cdc.gov/std/stats16/CDC_2016_STDS_Report-for508WebSep21_2017_1644.pdf.
7. CDC, Selected STDs by age, race/ethnicity, and gender, 1996–2014 request, no date, https://wonder.cdc.gov/std-race-age.html.
8. CDC, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, HIV and youth, 2018.
9. Brener N et al., Methodology of the Youth Risk Behavior Surveillance System—2013, Morbidity and Mortality Weekly Report, Vol. 62, No. RR-1.
10. CDC, Division of Adolescent and School Health, Adolescent and school health: YRBSS methods, 2018, https://www.cdc.gov/healthyyouth/data/yrbs/methods.htm.
11. CDC, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Software for Analysis of YRBS Data, 2018, https://www.cdc.gov/healthyyouth/data/yrbs/pdf/2017/2017_YRBS_analysis_software.pdf.
12. CDC, National Center for Chronic Disease Prevention and Health Promotion, Effectiveness of family planning methods, no date.
13. Charlton B et al., Sexual orientation differences in teen pregnancy and hormonal contraceptive use: an examination across two generations, American Journal of Obstetrics & Gynecology, 2013, 209(3):204.e1–204.e8, doi:10.1016/j.ajog.2013.06.036.
14. Schalet AT et al., Invited commentary: broadening the evidence for adolescent sexual and reproductive health and education in the United States, Journal of Youth and Adolescence, 2014, 43(10):1595–1610.
15. Jackson A et al., Racial and ethnic differences in women’s preferences for features of contraceptive methods, Contraception 93(5):406–411.
16. Dehlendorf C et al., Racial/ethnic disparities in contraceptive use: variation by age and women’s reproductive experiences, American Journal of Obstetrics & Gynecology 210(6):526-e1–9, doi:10.1016/j.ajog.2014.01.037.
Suggested Citation
Witwer E, Jones R and Lindberg L, Sexual Behavior and Contraceptive and Condom Use Among U.S. High School Students, 2013–2017, New York: Guttmacher Institute, 2018.
Acknowledgments
This report was prepared by Elizabeth Witwer, Rachel Jones and Laura Lindberg, all of the Guttmacher Institute. John Thomas edited the report, and Michael Moran designed the graphics and layout. Research support was provided by Cynthia Beavin and Isaac Maddow-Zimet. Heather Boonstra, Jesse Boyer, Amy Lieberman and Rebecca Wind provided valuable comments and suggestions.