This report examines the need for, impact of and cost of fully investing in sexual and reproductive health care—services that together ensure people can decide whether and when to have children, experience safe pregnancy and delivery, have healthy newborns, and have a safe and satisfying sexual life. It focuses on the need for contraceptive services, maternal and newborn care, abortion services and treatment for the major curable STIs among women of reproductive age (15–49) in 132 low- and middle-income countries. The report’s goal is to illustrate for national and local governments, the private sector and international development partners the magnitude of investments needed to expand and improve essential sexual and reproductive health services.
Adding It Up: Investing in Sexual and Reproductive Health 2019

- Executive Summary
- 1. Purpose, Overview and Methods
- 2. Contraceptive Services
- 3. Pregnancy-Related and Newborn Health Services
- 4. Combined Investment in Contraceptive Services and Essential Care for Pregnant Women and Newborns
- 5. Contraceptive, Pregnancy-Related and Newborn Care for Adolescents
- 6. Additional Sexual and Reproductive Health Services
- 7. Conclusions
- REFERENCES
Author(s)
Elizabeth A. Sully, Ann Biddlecom, Jacqueline E. Darroch, Taylor Riley, Lori S. Ashford, Naomi Lince-Deroche, Lauren Firestein and Rachel MurroReproductive rights are under attack. Will you help us fight back with facts?
Executive Summary
Sexual and reproductive health care encompasses a broad range of services that ensure people can decide whether and when to have children, experience safe pregnancy and delivery, have healthy newborns, and have a safe and satisfying sexual life. These services are important investments both because they enhance individual well-being and allow people to exercise their sexual and reproductive rights, and because they have far-reaching benefits for societies and for future generations.
This report examines core services that women need and use during their reproductive years: contraceptive services, pregnancy-related care (including maternal health care and abortion services), newborn care and treatment for STIs. It identifies services that, if expanded and strengthened, could improve the health of women, their partners and their children. It focuses on low- and middle-income countries (LMICs) and, like prior Adding It Up reports, presents the need for, impacts of and costs associated with providing services at internationally defined standards of care. The report’s goal is to illustrate for national and local governments, the private sector and international development partners the investments needed to expand and improve sexual and reproductive health services, which are essential components of health care.
Unmet needs for services
New estimates for 2019 show that sexual and reproductive health services fall well short of needs in LMICs. Approximately 218 million women of reproductive age (15–49) in these countries have an unmet need for modern contraception—that is, they want to avoid a pregnancy but are not using a modern method. About half (49%) of pregnancies in LMICs—111 million annually—are unintended.
In addition, 127 million women give birth each year, and tens of millions of them do not receive adequate pregnancy-related and newborn health care.
- 50 million make fewer than four antenatal care visits
- 31 million do not deliver in a health facility
- 16 million do not receive the care they need following a major obstetric complication
- 13 million have newborns who do not receive needed care for major complications
Many women whose pregnancies do not end in a live birth also lack needed services.
- 2 million do not receive the care they need after experiencing a miscarriage
- 35 million have abortions in unsafe conditions
- 9 million do not receive the necessary care for complications after an unsafe abortion
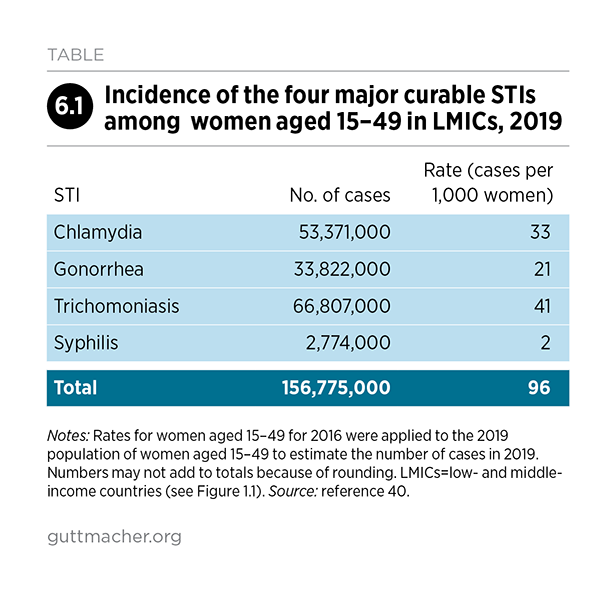
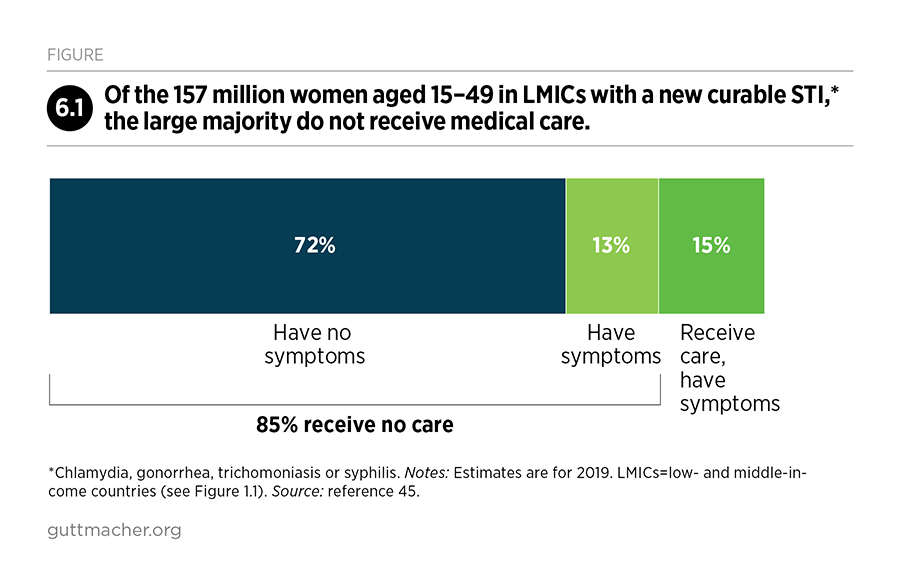
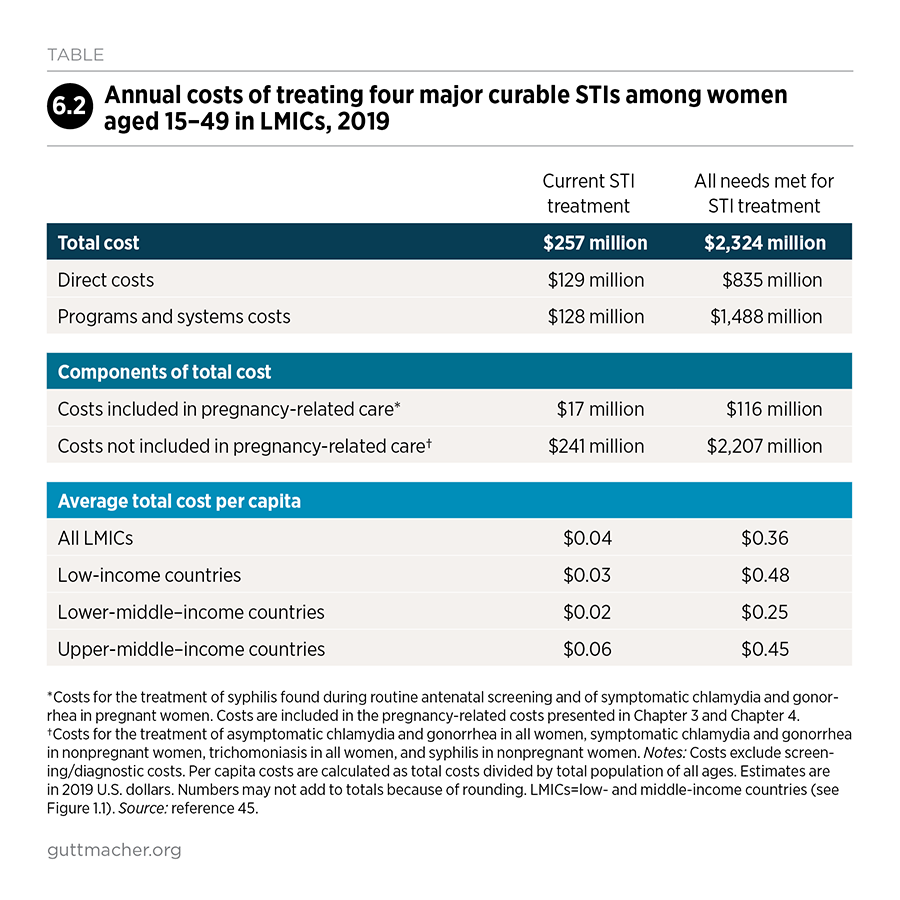
Furthermore, an estimated 133 million women of reproductive age in LMICs need but do not receive treatment for one of the four major curable STIs—chlamydia, gonorrhea, syphilis or trichomoniasis.
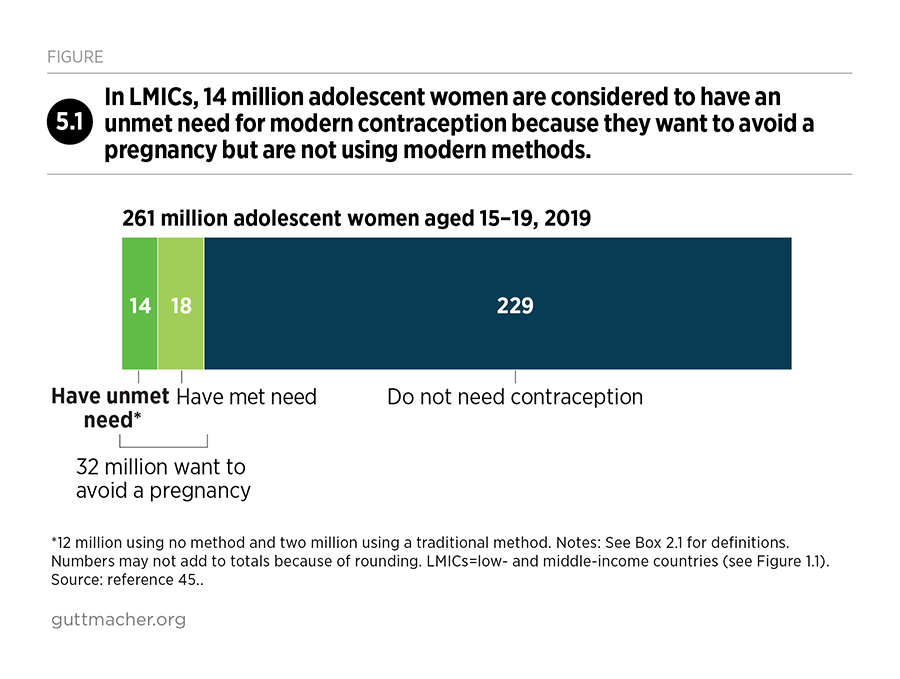
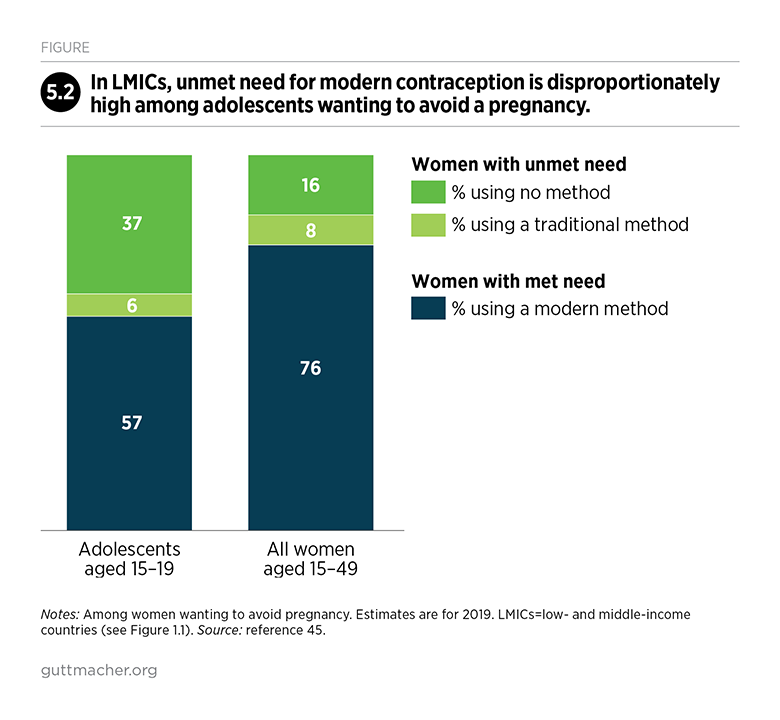
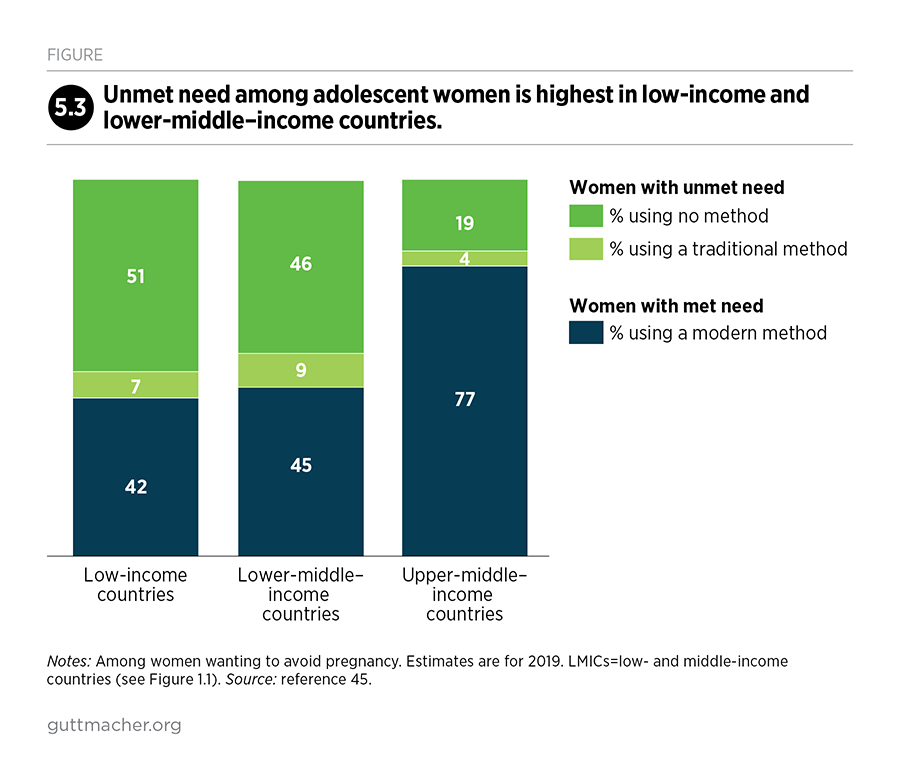
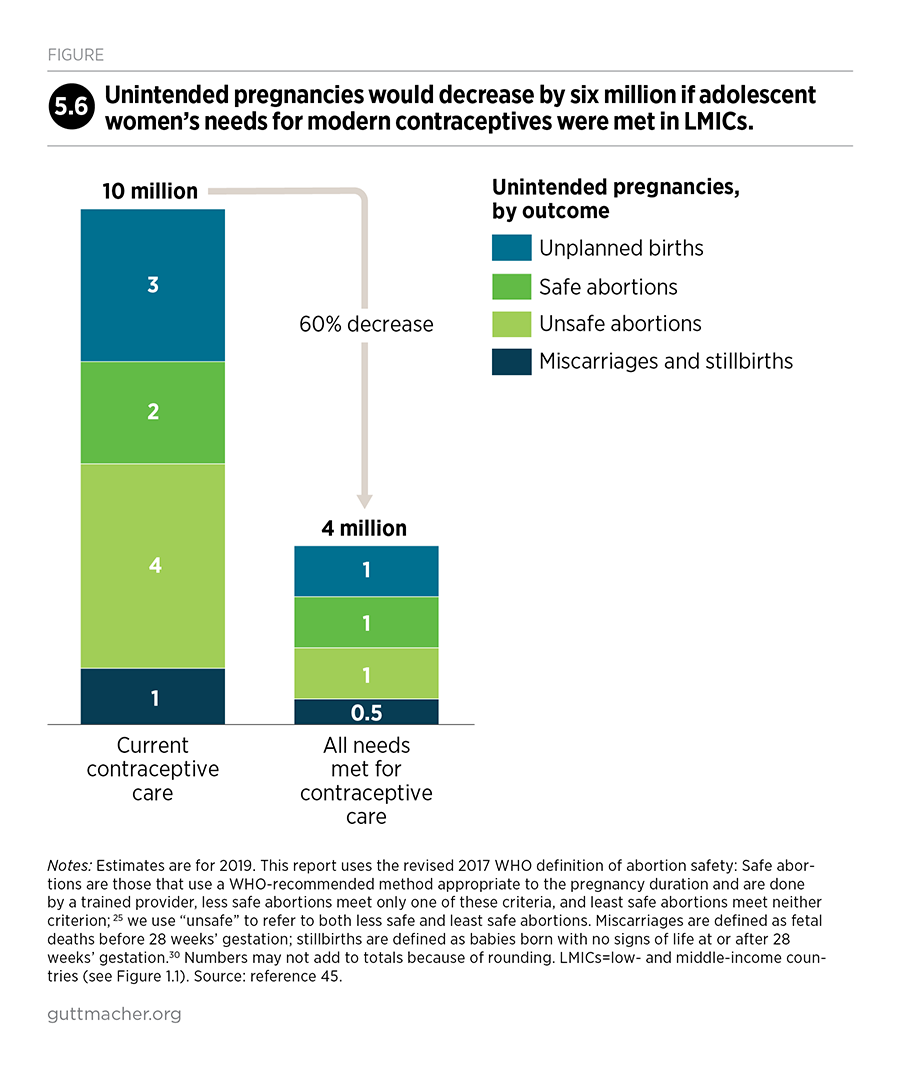
Adolescents, in particular, have substantial unmet needs for sexual and reproductive health care. For example, women aged 15–19 who want to avoid a pregnancy have much higher unmet need for modern contraception than do all women of reproductive age who want to avoid a pregnancy (43% vs. 24%). Adolescent women face many barriers to obtaining contraceptive care, including fear of exposing that they are sexually active (if they are unmarried) and social pressure to have a child (if they are married). Adolescents in LMICs have an estimated 21 million pregnancies each year, 50% of which are unintended.
Impacts of expanded services
If all women in LMICs wanting to avoid a pregnancy were to use modern contraceptives and all pregnant women and their newborns were to receive care at the standards recommended by the World Health Organization, the impacts would be dramatic:
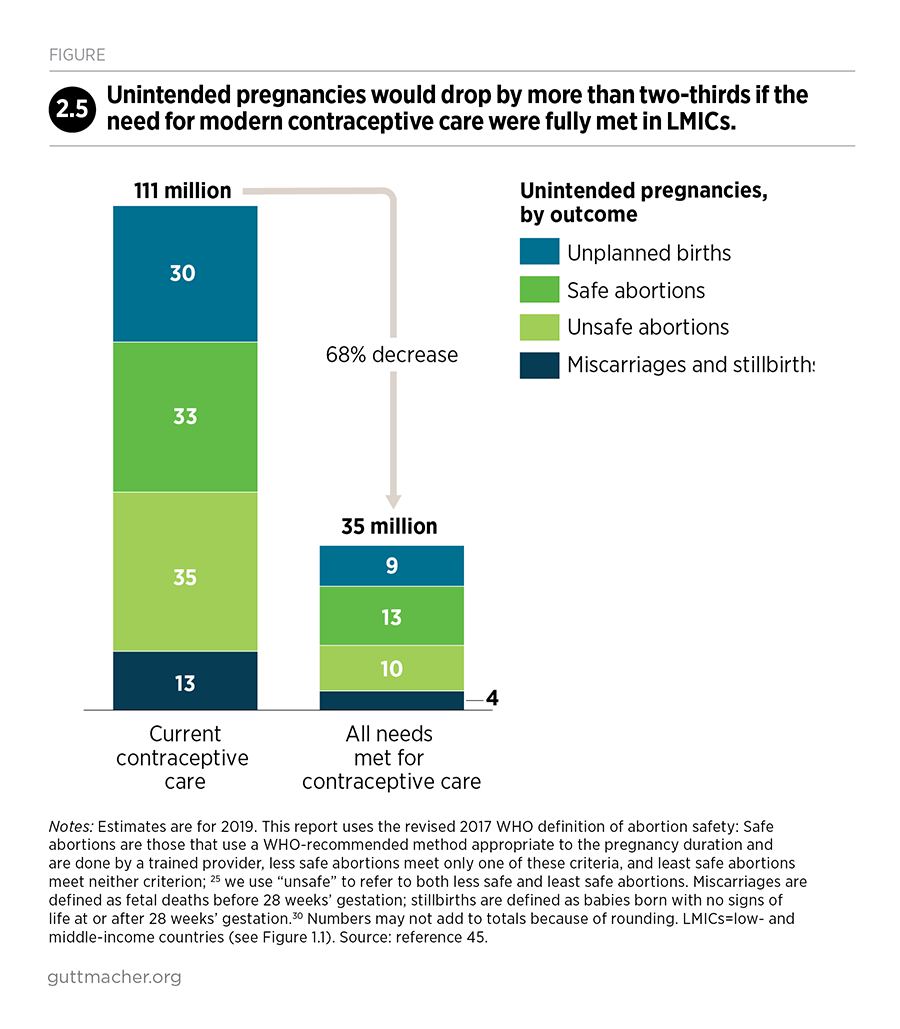
- Unintended pregnancies would drop by 68%
- Unsafe abortions would drop by 72%
- Maternal deaths would drop by 62%
Providing the recommended maternal and newborn care would also vastly improve newborn health. Newborn deaths would drop by 69%, and new HIV infections among babies six weeks and younger would drop by 88%.
In addition, if all women infected with chlamydia or gonorrhea were given effective and timely treatment, cases of pelvic inflammatory disease and infertility caused by these STIs would be eliminated.
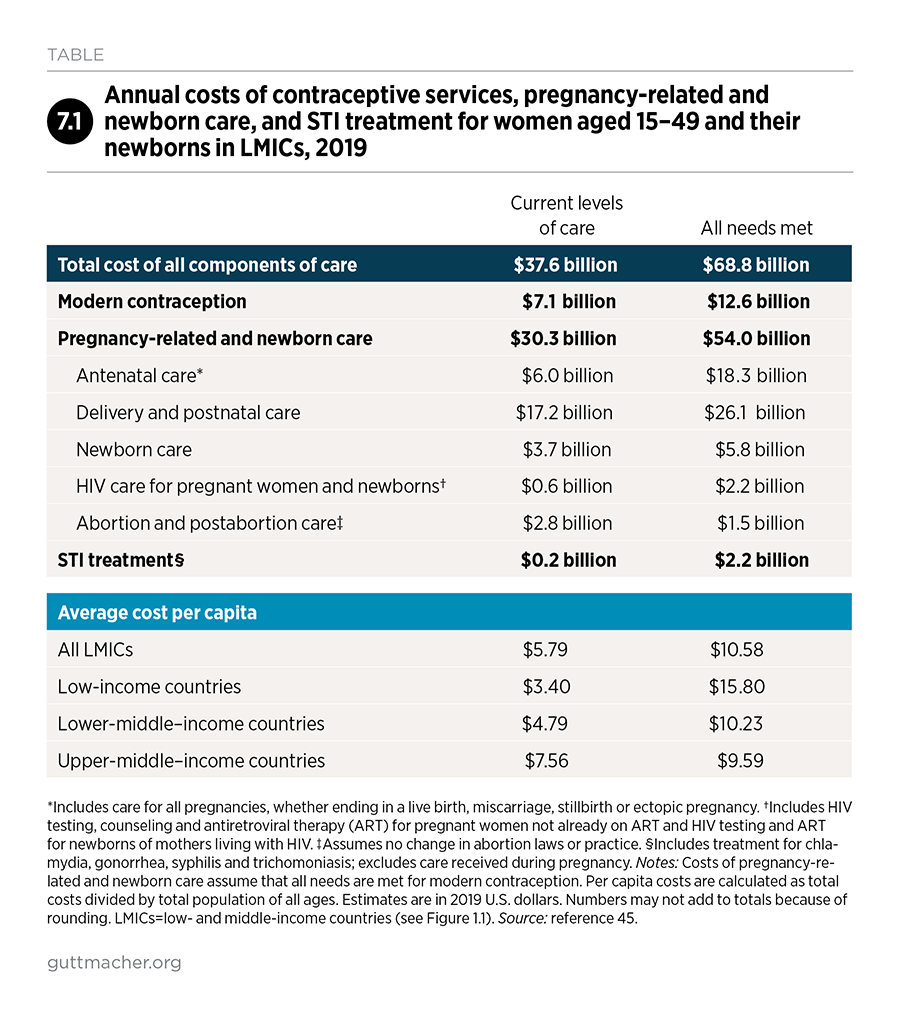
Total cost of a package of care
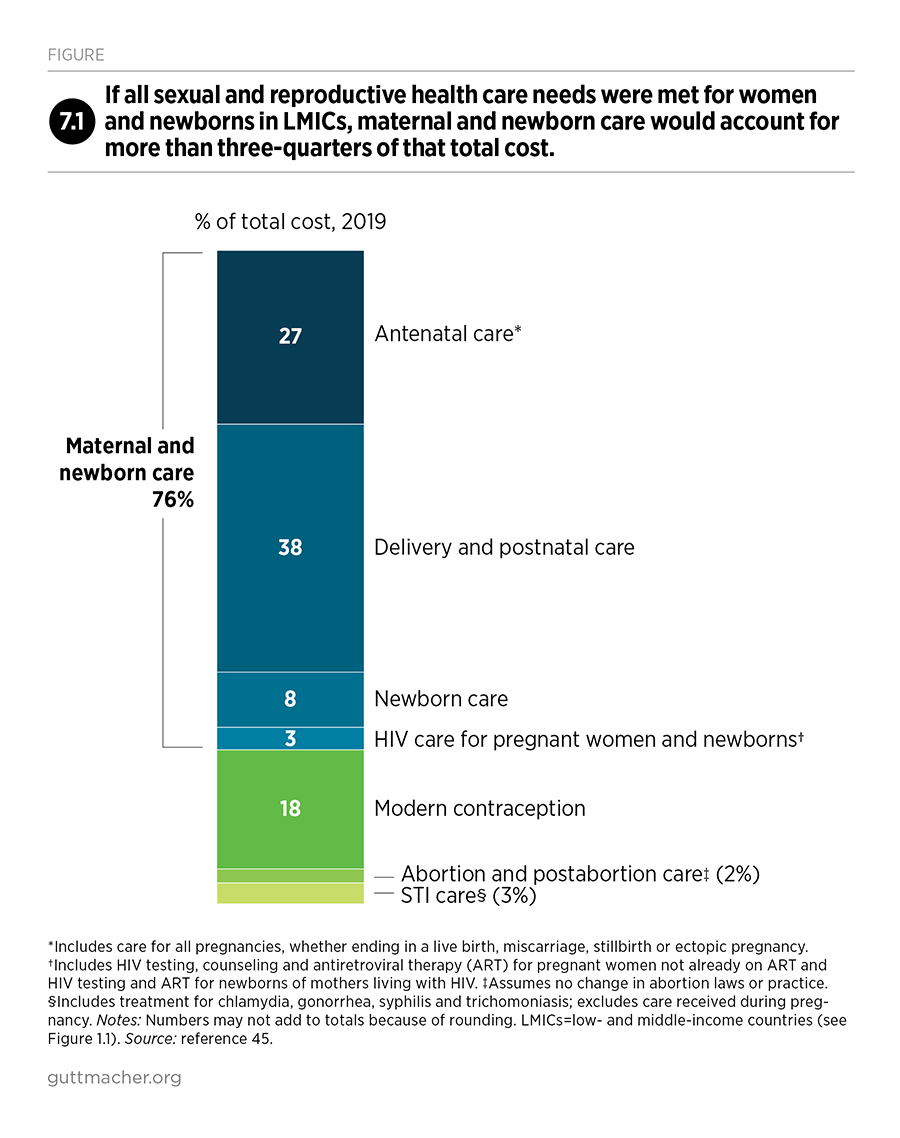
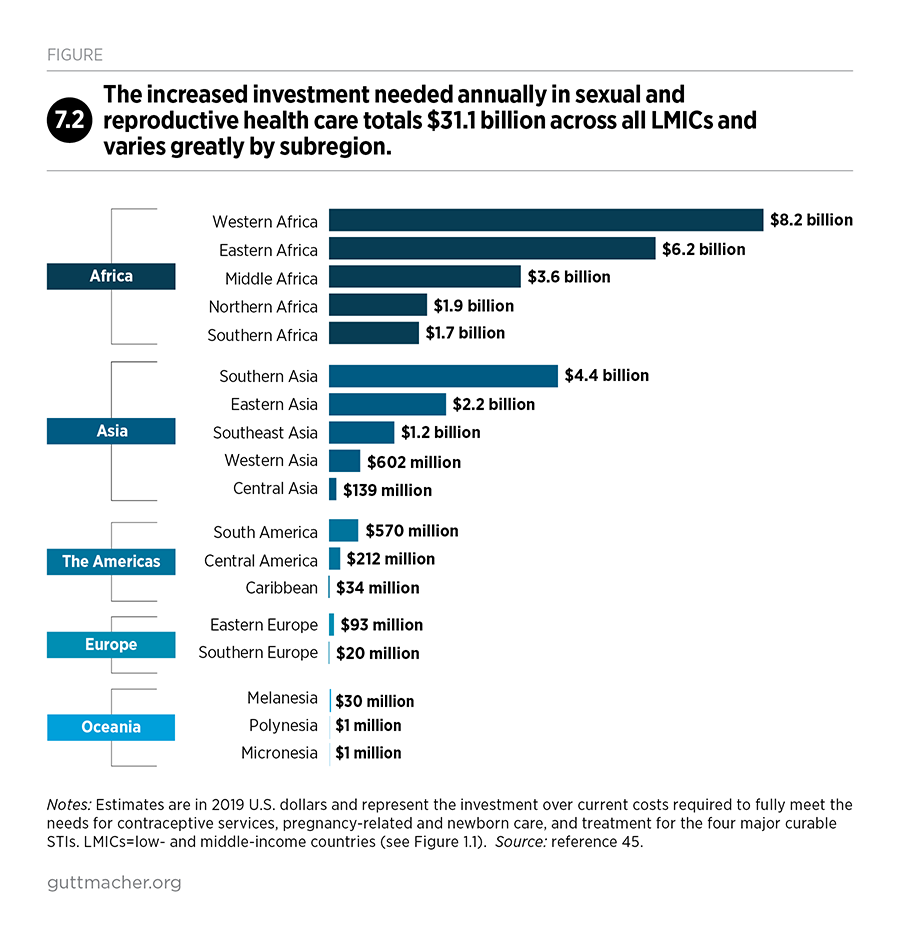
A package of care that would meet all women’s needs for modern contraception, pregnancy-related and newborn care, and treatment for the major curable STIs would cost $68.8 billion annually in 2019 U.S. dollars, or approximately $10.60 per capita (i.e., per total population in LMICs) per year. This represents an increase over current costs of about $4.80 per capita per year. This investment would improve the quality of services women currently receive and enable all women to receive the care they need.
The total recommended investment represents a $31 billion (83%) increase over current annual costs for LMICs. Two subregions, Sub-Saharan Africa and Southern Asia, account for more than three-quarters ($24 billion) of the total increase. Low-income countries, which are mostly concentrated in Sub-Saharan Africa, require the largest boost in resources—an increase from $3.40 to $15.80 per capita annually—because these countries’ unmet needs for services are the highest and the health systems supporting these services require the most expansion and improvement.
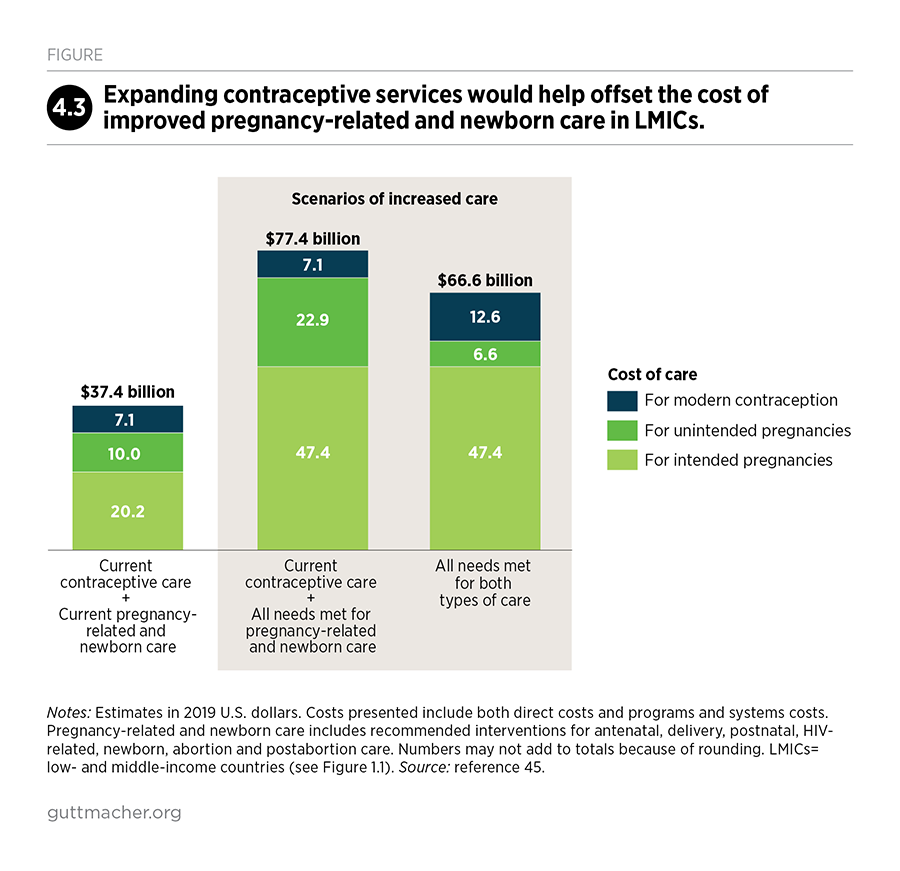
Importantly, fully investing in contraceptive services would result in a substantial decrease in unintended pregnancies, which would in turn reduce the need for pregnancy-related and newborn care. Every dollar spent on contraceptive services beyond the current level would reduce the cost of pregnancy-related and newborn care by three dollars. Thus, investing in both sets of services would result in cost savings of $11 billion compared with investing in pregnancy-related and newborn care alone.
Expanding and improving care
For approximately $10.60 per capita annually in LMICs, or about $4.80 more per capita than current costs, all women of reproductive age would receive the pregnancy-related and STI care that they need; all newborns would receive essential, lifesaving care during and just after birth; and women would receive the contraceptive services they need to be able to decide whether and when to have children. These gains would address substantial health burdens in LMICs and provide good value for money. In addition, the interventions that make up this service package have proven feasible to implement in diverse settings.
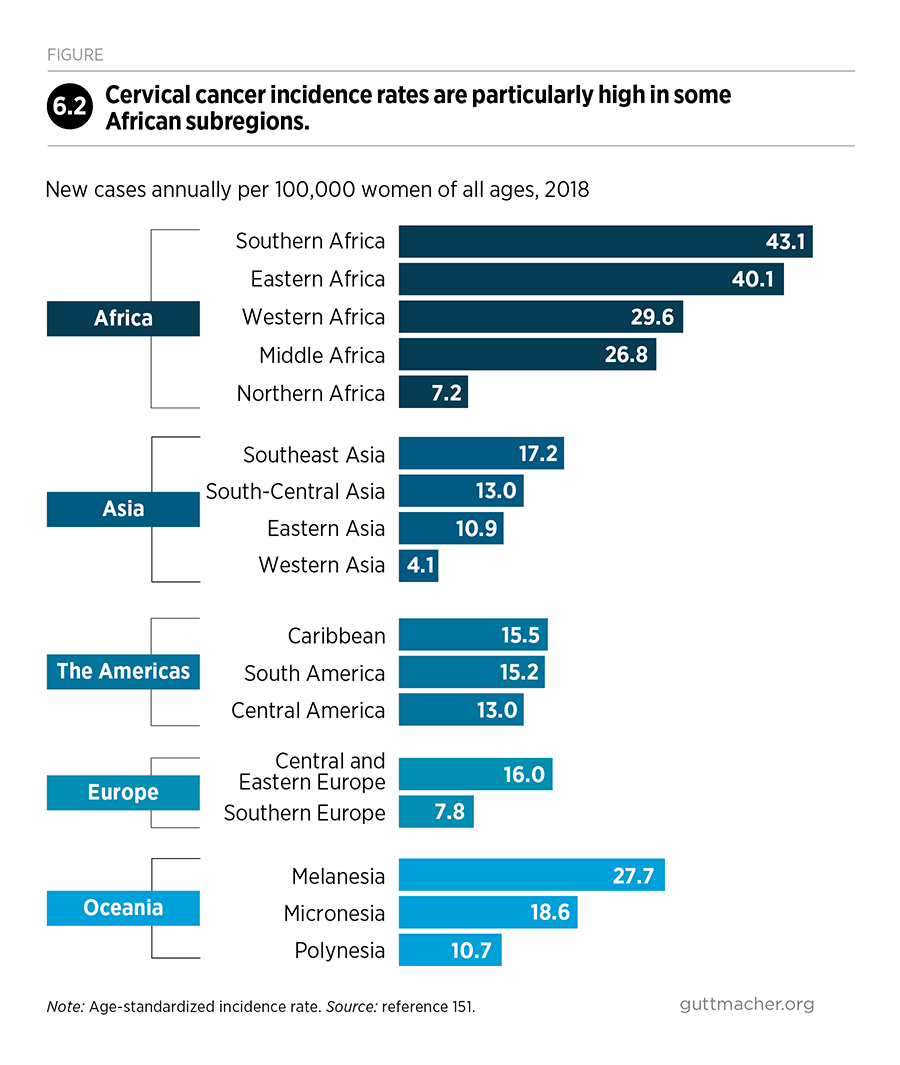
Investments are also critically needed to address other sexual and reproductive health needs, although they are not quantified in this report because the necessary data are lacking. Cervical cancer—which can be prevented with low-cost interventions—accounts for more deaths in many LMICs than do pregnancy-related complications. Nearly one in three women experience intimate partner violence, which has profound physical and mental health consequences. Young women continue to account for a disproportionate share of new HIV infections. People in humanitarian crises face heightened risks of STIs, unintended pregnancy and unsafe abortion, while services in these settings are uneven and usually inadequate. And infertility affects millions of couples worldwide, yet treatment is out of reach for those with modest incomes.
The funds for expanding and improving sexual and reproductive health care will need to come from a combination of sources that currently support services: national governments, nongovernmental organizations, international donor agencies and the individuals receiving care. Although financing models vary from one country to another, the objective of universal health coverage—which is now a widely accepted goal in the global health community—is to ensure access to care for the people most in need. In countries with high health burdens and limited domestic budgets, external donor funding and effective donor-recipient partnerships will continue to be necessary for expanding access to care.
The speed at which countries can expand provision of high-quality sexual and reproductive health care will vary greatly and will depend on their health system's starting point and capacity for making needed improvements. Not acting at all would result in high costs, financially, developmentally and from a human rights perspective. By investing in proven sexual and reproductive health interventions, countries can make greater progress toward their national health and development goals, and toward achieving the Sustainable Development Goals by 2030.
1. Purpose, Overview and Methods
Sexual and reproductive health and rights have far-reaching implications for individuals, families and society. Health and well-being depend on people’s ability to plan pregnancies and births; obtain high-quality care before, during and after a pregnancy; and prevent and treat HIV and other STIs. People who experience gender-based violence, infertility and reproductive cancers also rely on sexual and reproductive health care. A lack of access to these essential services jeopardizes individuals’ health and lives and, in turn, negatively affects families and social and economic development more broadly.
Recognizing the linkages between these fundamental aspects of individual health and broader development efforts, several global initiatives of the past decade have advanced parts of the sexual and reproductive health and rights agenda. For example, many of the 17 Sustainable Development Goals (SDGs)1—especially Goals 3, 4 and 5, which aim for improved health, education and gender equality, respectively—depend on improvements in sexual and reproductive health and rights. The health-related SDG targets for 2030 include satisfying people’s needs for modern contraception, reducing maternal and newborn deaths, and ending the HIV epidemic. To achieve these targets and reach the most disadvantaged populations, the SDGs also call for countries to attain universal health coverage, ensuring that quality services are accessible and affordable to everyone. These calls for improved sexual and reproductive health reflect the aims of other global initiatives, such as Family Planning 20202 and the UN’s Global Strategy for Women’s, Children’s and Adolescents’ Health.3
In 2018, the Guttmacher-Lancet Commission on Sexual and Reproductive Health and Rights outlined an essential package of sexual and reproductive health interventions to which all people should have access.4 This proposed package includes the key components of care promoted in the global initiatives described above, as well as often neglected elements, such as services for infertility and reproductive cancers. The commission also recognized that sexual and reproductive rights are linked with human rights, which countries have an obligation to uphold and which include rights to privacy, bodily autonomy and dignity, and to health care that is free of stigma, discrimination and coercion. This report builds on the commission’s evidence and recommendations by quantifying the need for specific sexual and reproductive health services in low- and middle-income countries (LMICs; Figure 1.1), and estimating the impacts and associated costs of expanding and improving these services.
The goal of this report is to guide decision makers, at the global, regional, national and local levels, in making investments in sexual and reproductive health services that would result in large returns for individuals and societies. Specifically, it examines services that women need and use during their reproductive years (15–49) and identifies services that, if expanded and strengthened, could improve women’s health, as well as that of their partners and children. The report builds on prior Adding It Up reports, which have provided periodic estimates of the need for, costs of and impacts of sexual and reproductive health services since 2003. Over time, the estimation methods have been refined, the package of care has expanded, and the countries included in the analysis have shifted slightly, but the purpose and approach have remained consistent.
The 2019 estimates
The 2019 estimates describe the need for and costs and impacts of the following sexual and reproductive health services for women of reproductive age in LMICs:
- Contraceptive services
- Pregnancy-related and newborn care, which includes maternal and newborn health care, safe abortion services and postabortion care
- Treatment for major curable STIs
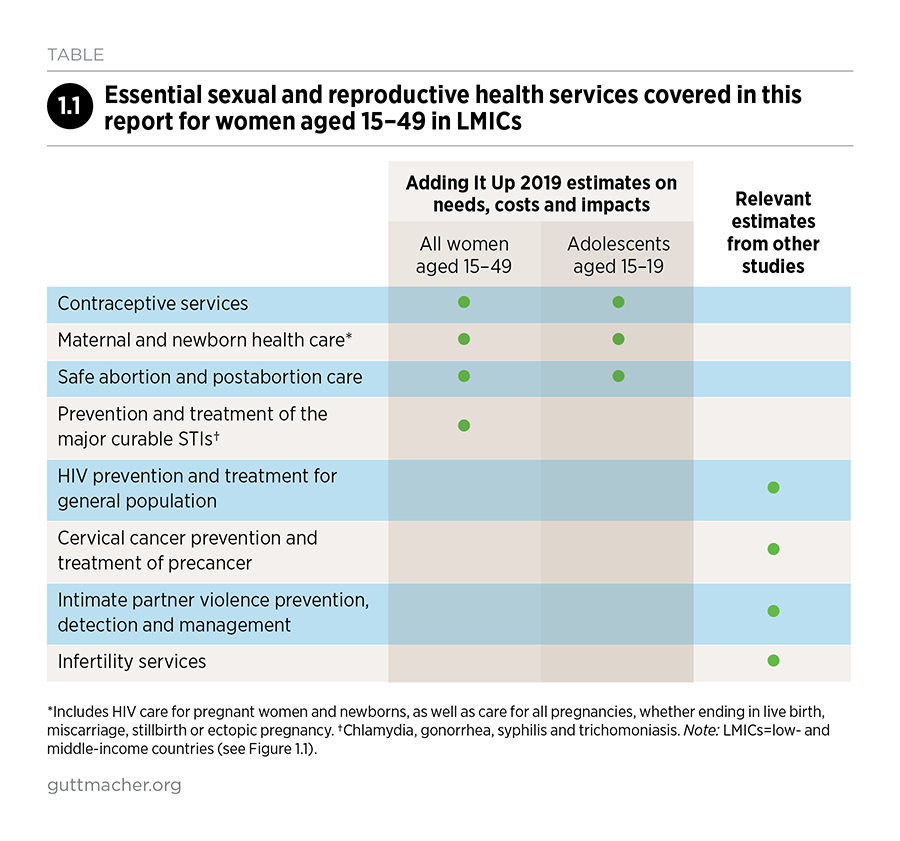
For these core services, sufficient data are available in LMICs to analyze unmet needs, service costs and impact systematically across countries (Box 1.1). For contraceptive care and pregnancy-related and newborn care, we discuss critical gaps in services and the improvements needed—in terms of both access and quality—as well as the specific needs of adolescents aged 15–19. In addition, we include findings on other sexual and reproductive health services that are not part of the 2019 estimates but for which the Guttmacher-Lancet Commission found ample evidence of need and effective interventions, and which should be considered vital elements of a continuum of care that supports people’s health throughout their reproductive lives (Table 1.1). We also draw attention to wealth disparities in health care utilization to help guide decision makers toward program designs and resource management strategies that support equitable access to services.
Although data on wealth disparities are widely available, data that speak to other important types of marginalization and discrimination are not. The groups of people for whom information is limited—and whose needs are often overlooked—include adolescents younger than 15, adults older than 49, sex workers, people who inject drugs, people with disabilities, racial and ethnic minorities, indigenous populations and LGBTQ individuals.4
This report does not examine men’s sexual and reproductive health needs independently from those of women because of the focus of the analysis and the data sources available. However, we identify the contexts in which women’s and men’s service needs overlap, such as the use of some contraceptive methods, prevention and treatment of STIs, and infertility services. We use the terms "women" and "men" to match the data available in nationally representative household surveys, although we recognize that not all people have binary gender identities.
Guide to this report
The report presents the following estimates as they relate to contraceptive services (in Chapter 2) and pregnancy-related and newborn care (in Chapter 3):
- Magnitude of service needs among women of reproductive age and their newborns
- Level and adequacy of current services
- Costs of current services and of full coverage of recommended care
- Impacts of current services and of meeting all service needs
Estimates are presented for LMICs as a group (132 countries) and, in some cases, by country-income group (low income, lower-middle income and upper-middle income)5 or by geographic regions and subregions.6 For some services, the report also examines disparities in care according to household wealth, using data from countries with recent national surveys. Appendix tables, available online, provide data for different country groupings (download above).
Chapter 4 presents estimates of the effects and cost savings that would result from fully meeting the needs for both contraceptive services and pregnancy-related and newborn care. In addition, beyond the direct, short-term impacts quantified here, we draw on other published research to describe the broad social and economic benefits that result from people being enabled to delay childbearing and have their desired number of children.
Chapter 5 focuses on adolescents aged 15–19, emphasizing that the foundation for good sexual and reproductive health begins early in life and exploring some of the long-term benefits that accrue from investing in adolescents’ sexual and reproductive health and rights.
Chapter 6 presents estimates on the need for and cost of treatment for major curable STIs among women of reproductive age. It also summarizes what we currently know about the need for—and in some cases, the costs associated with—other sexual and reproductive health services. These include the prevention and treatment of cervical cancer, HIV and infertility; services that respond to intimate partner violence; and sexual and reproductive health care in humanitarian crisis settings.
Chapter 7 summarizes the scope of need for sexual and reproductive health services and the efforts that will be required to make essential health service coverage a reality for everyone.
Box 1.1
How are the Adding It Up estimates generated?
Adding It Up is an ongoing project by the Guttmacher Institute that estimates the need for and the use, costs and impacts of sexual and reproductive health services in low- and middle-income countries (LMICs).7–12 The current study assesses the numbers of women of reproductive age (15–49) who need and receive contraceptive services, pregnancy-related and newborn services (defined as maternal and newborn care, including HIV-related services for pregnant women and their newborns, safe abortion services and postabortion care), and treatment for the most common curable STIs. It estimates the total costs of current services and of satisfying service needs for all women and newborns at internationally defined standards of care. This box briefly explains the methodology and data sources used. Additional details are available at https://www.guttmacher.org/report/adding-it-up-investing-in-sexual-repr….
To show the impacts of meeting women’s needs for contraceptive services and pregnancy-related and newborn care, this study compares current levels of service provision with the following hypothetical scenarios:
- No care: This scenario is used to show the health impact of current services by estimating outcomes if no contraceptive or pregnancy-related and newborn care were provided.
- Meeting the need for modern contraception and meeting the need for pregnancy-related and newborn care: These two scenarios show the costs and impacts of fully investing in just one set of services, assuming the other set remains at current levels.
- Fully meeting the need for both sets of services simultaneously: This scenario demonstrates how full provision of contraceptive services would reduce the need for pregnancy-related and newborn care, which would in turn result in greater impact and cost savings than investing in either set of services alone.
In addition, the study estimates the costs of current services for treating the four main curable STIs—chlamydia, gonorrhea, trichomoniasis and syphilis—as well as the impact and costs if all need for such care were fully met.
Costing
The analysis estimates the full cost to the health system of providing services, whether in public or private health facilities and regardless of who ultimately pays for the services. Both direct costs and indirect costs are included. Direct costs are estimated using a bottom-up, ingredients approach, meaning that the costs of resources required to provide a given service are added together to produce a total cost. These costs include personnel time; contraceptive commodities; medications, diagnostic tests and consumable supplies (referred to as drugs and supplies); and food costs during hospital stays. Personnel time includes the provision of information and counseling.
Indirect costs, referred to as programs and systems costs, are estimated by applying region-specific markup rates to direct costs. Programs and systems costs cover 10 categories: program management, staff supervision, monitoring and evaluation, human resources development, transport and telecommunications, health education and outreach, advocacy, infrastructure and equipment, commodity supply systems and health information systems. For scenarios in which needs for contraceptive or pregnancy-related and newborn care are fully met, we applied higher region-specific markup rates to reflect the increased resource requirements associated with expanding capacity and improving quality to meet international standards.
Estimates of the types and quantities of resources required to provide contraceptive services, pregnancy-related and newborn health care, and STI care are based on assumptions from the Lives Saved Tool (Spectrum Version 5.73)13 and the OneHealth Tool,14 supplemented by scientific literature, World Health Organization (WHO) policies and general recommendations, and expert review. Country-specific personnel salaries come from WHO-CHOICE personnel cost estimates from 201015 and have been inflated to 2019 levels. Contraceptive commodity costs are average prices for 2015–2018 and come from the Reproductive Health Interchange database.16 Nearly all prices for drugs and supplies are drawn from the United Nations Population Fund (UNFPA),17 UNICEF,18 Management Sciences for Health19 and IDA Foundation.20 The programs and systems costs are based on estimates from UNFPA.21
We present the cost for all scenarios as annual costs in 2019 U.S. dollars. Most of the sources we use to estimate direct costs for contraceptive commodities, drugs and supplies reflect public-sector prices. These may therefore underestimate costs somewhat, especially for countries relying heavily on private-sector care. For simplicity, we assume that the additional cost of meeting individuals’ needs is the same regardless of the number of people served (i.e., marginal costs remain constant and there are no economies of scale). Moreover, our estimates do not account for costs associated with addressing all barriers to the use of health services (within or outside of the health system), nor the costs of modifying services to meet certain groups’ specific needs. Finally, we assume in scenarios of increased service provision that the required investments and resulting gains are immediate—occurring in 2019. Using the same reference year for all scenarios facilitates comparison and makes it easier to illustrate the impacts of fully meeting all service needs. In practice, meeting all service needs requires expanding or improving health care infrastructure and training health care workers, and these steps would take time to achieve.
Demographic and health data sources
The 2019 estimates draw on the most recent data sources; numbers were adjusted to 2019 as needed. Nationally representative surveys of women aged 15–49 are the principal source of information for measures of women’s fertility preferences, contraceptive use, and receipt of pregnancy-related, newborn and STI care. These surveys include Demographic and Health Surveys, UNICEF Multiple Indicator Cluster Surveys, U.S. Centers for Disease Control Reproductive Health Surveys, and Performance Monitoring for Action Surveys, among others. We aligned the survey data on contraceptive use with the UN Population Division’s annual model-based estimates of the proportions of married and unmarried women using contraceptives and having unmet need in 2019.22
Population projections of women aged 15–49 and of the annual number of live births in 2019 are from the UN Population Division.6 Estimates of unintended pregnancy, abortion incidence and abortion safety are from the Guttmacher Institute, WHO and other authors, and are adjusted to 2019.23–29
Stillbirths are based on estimates by The Lancet Stillbirth Epidemiology Investigator Group.30 Miscarriages are estimated as a proportion of live births and abortions.31 Estimates of maternal deaths and their causes are from the UN Maternal Mortality Estimation Inter-Agency Group32 and the Institute for Health Metrics and Evaluation, respectively33 and data for newborns are from WHO.34
Estimates of the number of unintended pregnancies averted as a result of contraceptive use are based on age- and method-specific use-failure rates from a number of studies35–38 and a pregnancy rate for women who want to avoid a pregnancy but are using no method.39 We applied country-specific adjustment ratios to our estimates of unintended pregnancies to align them with a robust set of modeled estimates.24 The impacts of maternal and newborn health care are based on condition-specific effectiveness rates of components of pregnancy-related and newborn care in reducing maternal and newborn death, which come from the Lives Saved Tool.13
Estimates of new infection rates for the four main curable STIs in women are from WHO.40 We multiply the rates by the population of women aged 15–49 in each country to estimate the total annual number of new infections for all four STIs combined.41
Presentation of results and missing data
The report shows cost and impact estimates for LMICs as a whole; by income grouping, as defined by the World Bank;5 and by geographic region and subregion, as defined by the UN Population Division.6 Totals reflect the sum of individual country estimates, and percentages represent weighted averages for countries in that grouping. For most countries where health-related data are unavailable, we use the subregional or regional weighted average. Five countries or territories classified as LMICs are excluded from the analysis because the UN does not publish population or births data for them.* Estimates for a number of country groupings, such as UNFPA regions, can be found in the appendix tables (download above).
Comparability with prior reports
While the basic Adding It Up approach has remained consistent over time, each update of the estimates involves adjusting the project’s scope and methodology; therefore, estimates from different reports should not be used as a time series. Whereas prior reports presented totals for developing regions, which are defined geographically, this report presents estimates for LMICs. In making this change, we exclude the approximately 3% of women of reproductive age in developing regions who live in high-income countries. In addition, we include LMICs in Eastern and Southern Europe, which were excluded from prior reports that focused on developing regions.
Several other changes also prevent comparisons with prior reports. These include adjustments in our estimates of contraceptive needs and use to align with those of the UN Population Division,22 new estimates of abortions and unintended pregnancies,24 and many updated sources of information.
2. Contraceptive Services
Contraception has long been a cornerstone of sexual and reproductive health care because it enables people to choose whether and when to have children. By doing so, it can save women’s and children’s lives and enhance their health and well-being. Because of its wide-ranging and long-term benefits for women, their families, their communities and their countries’ social and economic development, contraception is one of the most cost-effective investments in health.42–44
Contraceptive use has increased dramatically worldwide over the last four decades,22 as couples have increasingly chosen to have fewer children and as modern contraceptive methods have become widely available through public-sector family planning programs, nongovernmental organizations, and private-sector clinics and pharmacies. However, a substantial proportion of women who want to avoid a pregnancy—whether to postpone, space or stop childbearing—are not using a modern method. In some of the poorest countries, the quality and accessibility of contraceptive services remain weak, even while the desire for smaller families grows.4
This chapter presents estimates of the need for and use of modern contraceptives in low- and middle-income countries (LMICs) in 2019, defining unmet need and describing the service improvements required to meet women’s needs. We show the impacts of modern contraceptive use, both at the current level and in a scenario in which all women who need modern methods use them. We then present cost estimates for both of these contraceptive service scenarios. The costs and impacts are presented as annual estimates for 2019, although, in reality, the necessary service improvements would occur over time.
The need for contraception
Worldwide, women have an average of 2.5 children (in 2015–2020), ranging from 1.7 in high-income countries to 4.5 in low-income countries.6 Even women on the upper end of this range spend most of their reproductive years wanting to avoid a pregnancy and therefore needing effective means to prevent pregnancy.
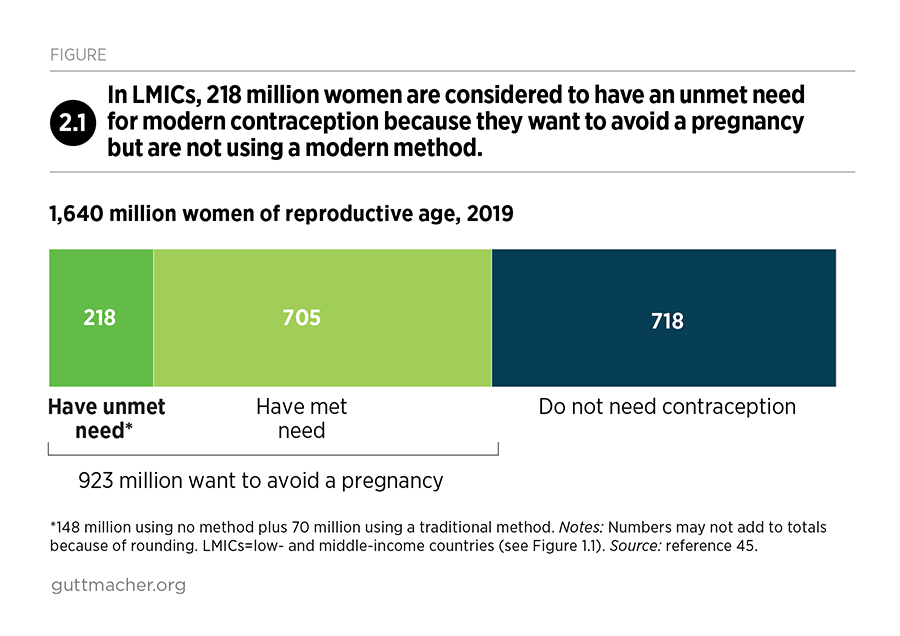
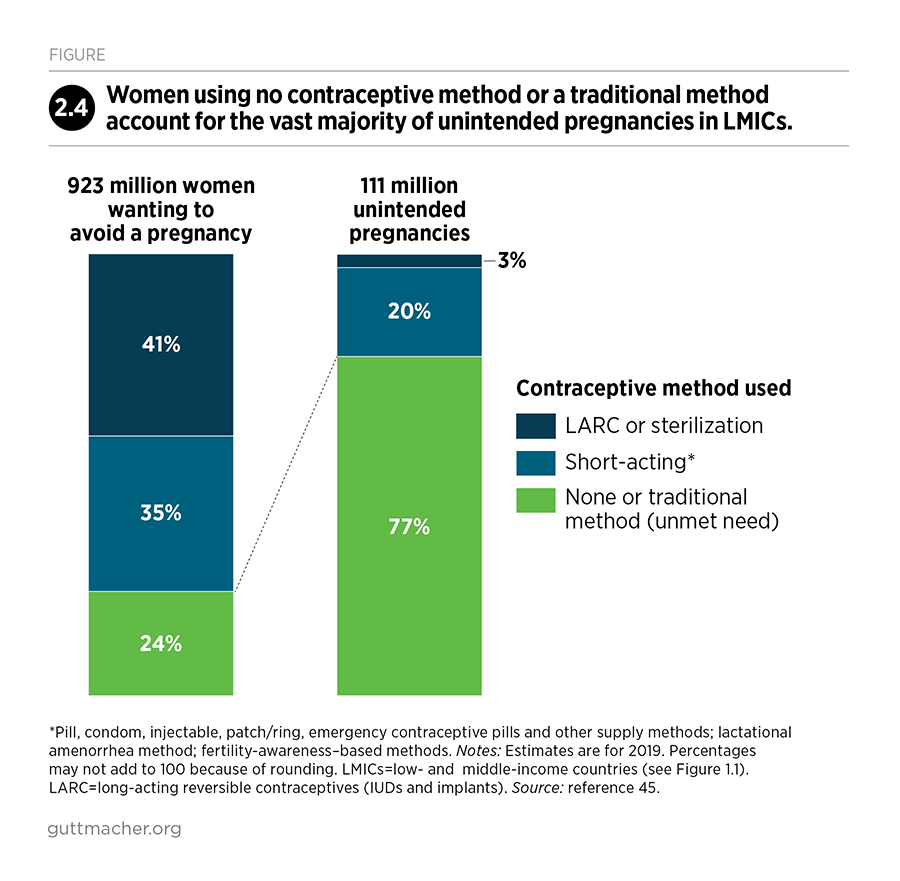
As of 2019, more than half of the 1.6 billion women of reproductive age living in LMICs want to avoid a pregnancy (Figure 2.1).45 Among these 923 million women who do not want to become pregnant, about three-quarters (705 million) use modern contraceptives and one-quarter (218 million) do not. This last group is considered to have an unmet need for modern contraception—that is, they want to avoid a pregnancy but are either using a traditional method or are using no contraceptive method at all (Box 2.1). Another 718 million women do not currently need contraception because they are unmarried and not sexually active, are not able to become pregnant, have recently had a planned birth, currently have an intended pregnancy or want to have a child in the next two years.
Box 2.1
Defining the need for modern contraception
In this report, women wanting to avoid a pregnancy are those aged 15–49 who fall into any of the following categories:
- Women using a contraceptive method, either traditional or modern
- Women who are married or are unmarried and sexually active, are able to become pregnant, and do not want a child in the next two years or at all
- Women who are pregnant and identify their pregnancy as unintended
- Women experiencing postpartum amenorrhea after an unintended pregnancy
In this definition, currently married women are assumed to be sexually active. Unmarried women are considered sexually active if they have had sex in the 30 days prior to the survey. This represents a departure from prior Adding It Up reports (which classified unmarried women as sexually active if they had had sex in the three months prior to the survey) and aligns with the definition of sexually active used by United Nations Population Division.†46 Women whose current pregnancy was unintended and women with postpartum amenorrhea after an unintended pregnancy are included in this definition because their experience indicates that they wanted to avoid becoming pregnant at some point in the last year. These groups help to complete the picture of the total number of women wanting to avoid pregnancy in a given year.
Women with unmet need for modern contraception are those who want to avoid a pregnancy but are currently using a traditional contraceptive method or are using no method. This analysis focuses on the need for modern methods because traditional methods, although more effective than nonuse, are less effective than modern methods and thus place users at an elevated risk of unintended pregnancy.35 (Note that some sources do not consider women using traditional methods as having an unmet need for contraception.47) This report expresses unmet need as a proportion of women wanting to avoid a pregnancy.
Modern contraceptive methods are defined in this analysis as any of the following:
- Permanent methods (female and male sterilization)
- Long-acting reversible methods (implants and IUDs)
- Short-acting methods (hormonal pills, injectables, male and female condoms, emergency contraceptive pills, patches, rings, diaphragms, vaginal spermicides and other supply methods)
- Lactational amenorrhea method, which involves exclusive breast-feeding for up to six months postpartum
- Two fertility awareness-based methods: Standard Days Method and TwoDay Method
Traditional methods include periodic abstinence, withdrawal, abstinence and breast-feeding.
Women whose need for modern contraception is met are those women of reproductive age who want to avoid a pregnancy and are using a modern method. The proportion of women whose need for contraception is satisfied with modern methods is a Sustainable Development Goal indicator48 used to measure progress toward the target of universal access to sexual and reproductive health services by 2030.1
Unmet need for modern contraception
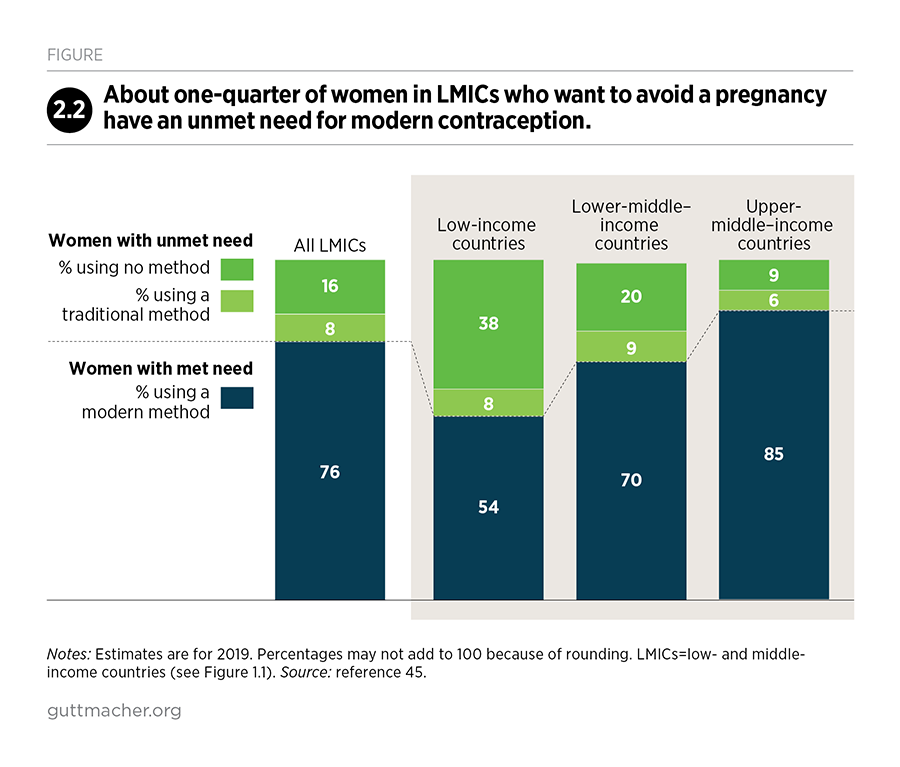
Among women in LMICs who want to avoid a pregnancy, 24% have an unmet need for modern contraception (Figure 2.2).45 Unmet need is highest in low-income countries, where nearly half (46%) of women who want to avoid a pregnancy are not using a modern method. Disparities also exist by age-group, socioeconomic status and urban-rural residence.49,50 For example, the proportion of women wanting to avoid pregnancy who have an unmet need is much higher among adolescent women aged 15–19 (43%) than among all women of reproductive age (see Chapter 5 for more information on adolescents’ sexual and reproductive health needs).
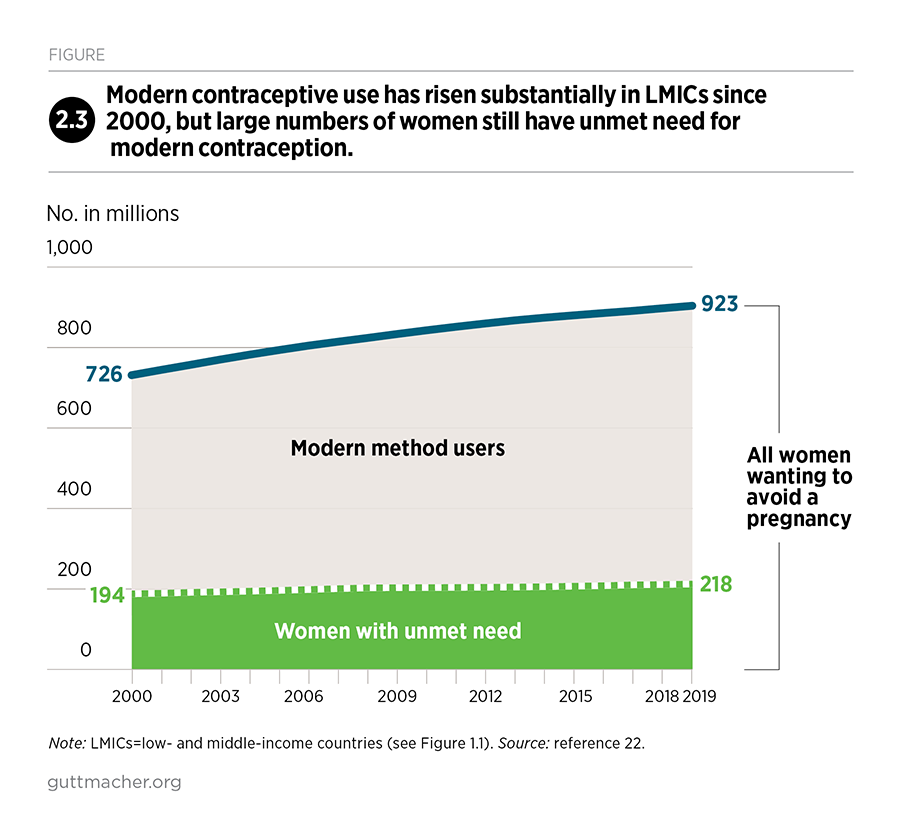
Trend data from the United Nations Population Division reveal that both the number of women wanting to avoid a pregnancy and the number of women using modern contraceptives has risen substantially since 2000 (Figure 2.3).22 However, population growth and the increased desire to avoid pregnancy have outpaced increases in contraceptive use. As a result, the number of women with an unmet need for modern methods has also increased.
Understanding and addressing unmet need
In LMICs as a whole, women with an unmet need for modern contraception are divided nearly evenly between women who want to postpone (or space) births and those who want to stop having children or avoid childbearing altogether.45 However, in low-income countries, unmet need is twice as high among women who want to space births as among those who want to limit births—suggesting that policies and programs should emphasize reaching women who wish to prevent pregnancy in the near term but who want to have a child in the future. Whether women wish to postpone or stop childbearing may affect what contraceptive methods they choose and what types of methods providers make available to them. Women wishing to delay a birth tend to rely on short-acting methods such as condoms, pills and injectables, while those wanting to have no more children tend to rely on sterilization or a long-acting reversible method, such as an implant or IUD. However, women who want to postpone births can also use long-acting reversible methods, which can be removed and are among the most effective methods for preventing unintended pregnancies.
Reports on family planning commonly say that women have unmet need because they lack access to contraceptive services, but that is only one of many reasons for not using contraceptives.51 When women who want to avoid a pregnancy are asked why they do not use contraceptives, many have concerns about their health or the side effects of methods, believe that they are not likely to become pregnant, or state that they or their family are opposed to contraception.52 Provider bias, particularly unwillingness to supply methods to young, unmarried or childless women, serves as a further barrier to contraceptive use and to reproductive autonomy more broadly.53
Moreover, research has shown that many women who use reversible modern methods do so inconsistently or discontinue use because they are not satisfied with the method, are concerned about the side effects or have trouble getting supplies.54 Data for 33 LMICs show that an average of 20% of users of short-acting methods who want to avoid pregnancy discontinue use within the first year.2 In contrast, only 11% of IUD users and 8% of implant users who want to avoid becoming pregnant discontinue use in the first year; though, these methods are harder to discontinue because they require removal by a health professional. Women who stop using contraceptives account for a significant proportion of overall unmet need for modern methods. In a 2013 study of 34 LMICs, women who discontinued method use and subsequently had unmet need accounted for 38% of overall unmet need. To reduce unmet need, offering high-quality services, including counseling, to women with met need is as important as serving new users.55
The motivations and circumstances that affect contraceptive use are wide-ranging and change over the course of people’s reproductive lives. Service providers should, therefore, offer all clients a range of contraceptive options, offer counseling to help them select the method or methods that best fit their current situation, and support them in using methods consistently and correctly. In addition, helping people switch methods when they want, or use methods that can prevent both pregnancy and STIs, including HIV, are important ways of matching contraceptive use to people’s specific needs and situations.
Over the long term, new developments in contraceptive technologies will expand contraceptive choices and the ways in which methods are delivered, thereby addressing many concerns that currently discourage people from using a method.4 Some of the new options under development include hormonal and nonhormonal male contraceptive methods, which would give men more options to control their own fertility and increase protection against unintended pregnancy if both partners are using a method.56 Currently, the majority of women wanting to avoid a pregnancy are using female-controlled modern contraceptive methods, and only 17% are using a method that requires their partner’s involvement (male condoms, male sterilization or fertility awareness-based methods).45 Evolving technology may facilitate a more active role for men in preventing pregnancy.
Improved service provision and new methods, although important and necessary, will not be enough to address unmet need within many communities. Generating demand—that is, increasing awareness of the benefits of contraceptive services and motivating individuals to use them—is also important, especially in areas where access to accurate information about contraception is limited. Mass media campaigns, social and community mobilization, and financial incentive schemes are all effective approaches to increase the demand for and use of modern contraceptive methods.57,58
Some barriers to contraceptive use originate outside the health system, including women’s lack of education or empowerment, which stem from gender discrimination and inequity in society. Fundamental changes in social structures and norms are necessary to address these deep-seated barriers. Improving the quality of sexual and reproductive health information and services can play a vital role in helping women overcome some of these barriers, by contributing to care that upholds and protects women’s rights to voluntary and informed contraceptive choice (see Box 2.2). These improvements would be consistent with fulfilling women’s human rights.
Box 2.2
Critical elements of quality in contraceptive services
According to the World Health Organization (WHO), the following human rights principles and standards apply to contraceptive services: nondiscrimination; availability, accessibility, acceptability and quality of information and care; informed decision-making, privacy and confidentiality for clients; community participation in program design, implementation and monitoring; and accountability in the provision of information and services.59 The international sexual and reproductive health community, including initiatives such as Family Planning 2020,60 has widely agreed to these principles because they are consistent with the fundamental right of individuals to decide freely whether and when to have children, and how many children to have.
Quality of care is a crucial principle. In contraceptive services, it implies more than skilled providers and adequate supplies of methods. It also includes focusing on clients’ concerns and providing effective counseling, which can promote uptake of services and help to ensure that people use their chosen method or methods effectively. WHO guidance defines quality services as including the following:59
- Choice among a wide range of contraceptive methods
- Evidence-based information on the effectiveness, risks and benefits of methods
- Technically competent health workers
- Provider-user relationships based on respect for informed choice, privacy and confidentiality
- Provision of the appropriate array of services in one location (e.g., offering long-acting reversible contraceptives, counseling on side effects, and services for insertion and removal at the same facility)
The guidance also recommends that contraceptive services incorporate quality-assurance processes, including medical standards of care and client feedback, and that health care personnel receive ongoing training on the delivery of contraceptive information and services.
Impacts of modern contraceptive use
Out of 228 million pregnancies occurring each year in LMICs (as of 2019), an estimated 111 million (49%) are unintended.45 Unintended pregnancies occur when couples either do not use a contraceptive method or experience contraceptive failure (due to inconsistent or incorrect use, or due to failure of the method itself). The chance of unintended pregnancy is greatly elevated when no modern method is used. Among women who want to avoid a pregnancy, 24% have an unmet need (because they are using either no method or a traditional method); 35% rely on short-acting methods such as pills, injectables and condoms; 17% use long-acting reversible contraceptives; and 24% rely on sterilization.
Of the 111 million unintended pregnancies, the majority (77%) occur among the 24% of women who want to avoid a pregnancy but are not using modern contraceptives (Figure 2.4). Another 20% of unintended pregnancies occur among those using short-acting contraceptives. Only 3% occur among the women who rely on sterilization or long-acting reversible contraceptives.
These 111 million unintended pregnancies result in the following estimated outcomes:
- 30 million unplanned births
- 69 million abortions, of which 35 million are unsafe‡
- 12 million miscarriages§
- 1 million stillbirths**
Current levels of contraceptive care are essential to maintain, because unintended pregnancies would be much higher in the absence of any modern contraceptive use. In 2019, 705 million women in LMICs used modern methods, thus preventing 376 million unintended pregnancies that would have occurred if these women used no method.45 By preventing these unintended pregnancies, current modern method use averts the following outcomes (data not shown):
- 79 million unplanned births
- 256 million abortions, of which 100 million would have been unsafe
- 39 million miscarriages
- 2 million stillbirths
If all 218 million women in LMICs with unmet need for modern contraceptives were to adopt and use them, unintended pregnancies would drop dramatically, from 111 million to 35 million per year (Figure 2.5).45 Unintended pregnancies would not be eliminated completely because some users would experience contraceptive failure—especially those using methods such as condoms and pills that rely on correct and consistent use. The drop in unintended pregnancies would result in the following outcomes:
- 21 million fewer unplanned births each year
- 46 million fewer abortions, of which 26 million would be unsafe
- 8 million fewer miscarriages
- 0.7 million fewer stillbirths
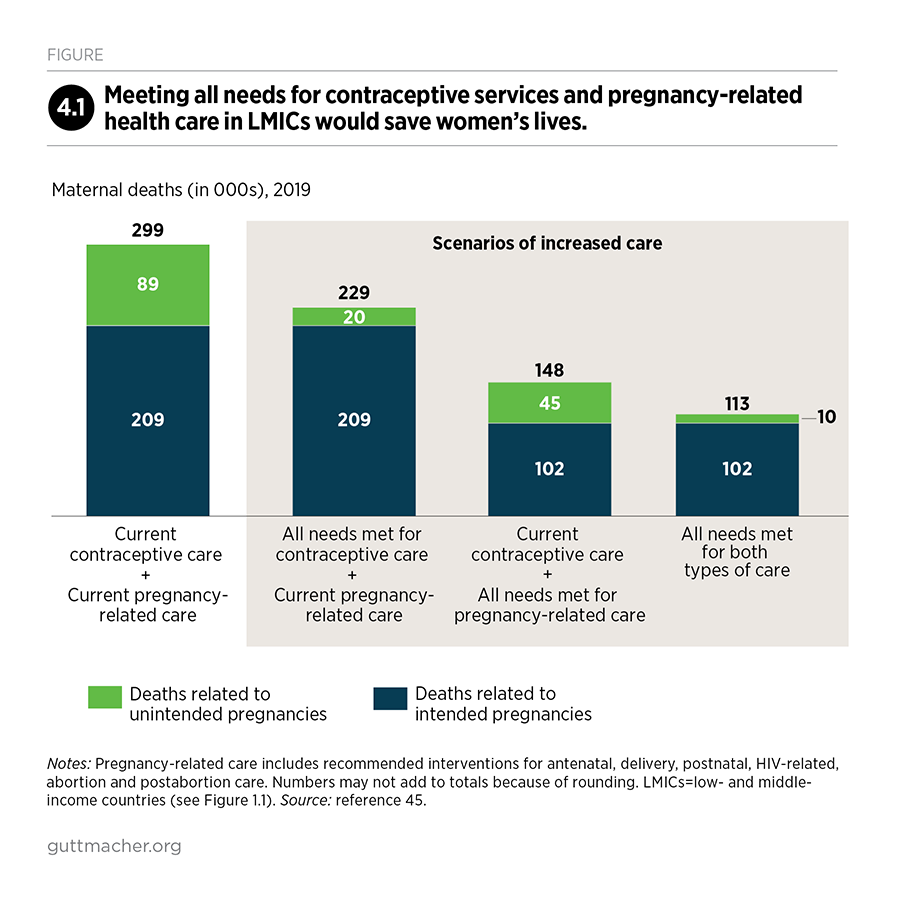
The benefits of averting these unintended pregnancies would be substantial. Compared with the current situation, fulfilling all need for modern contraception would result in 70,000 fewer maternal deaths each year—a 23% decline, even without improvements in pregnancy-related care. The additional reduction in maternal deaths that would result from improving care for pregnant women is discussed in Chapters 3 and 4.
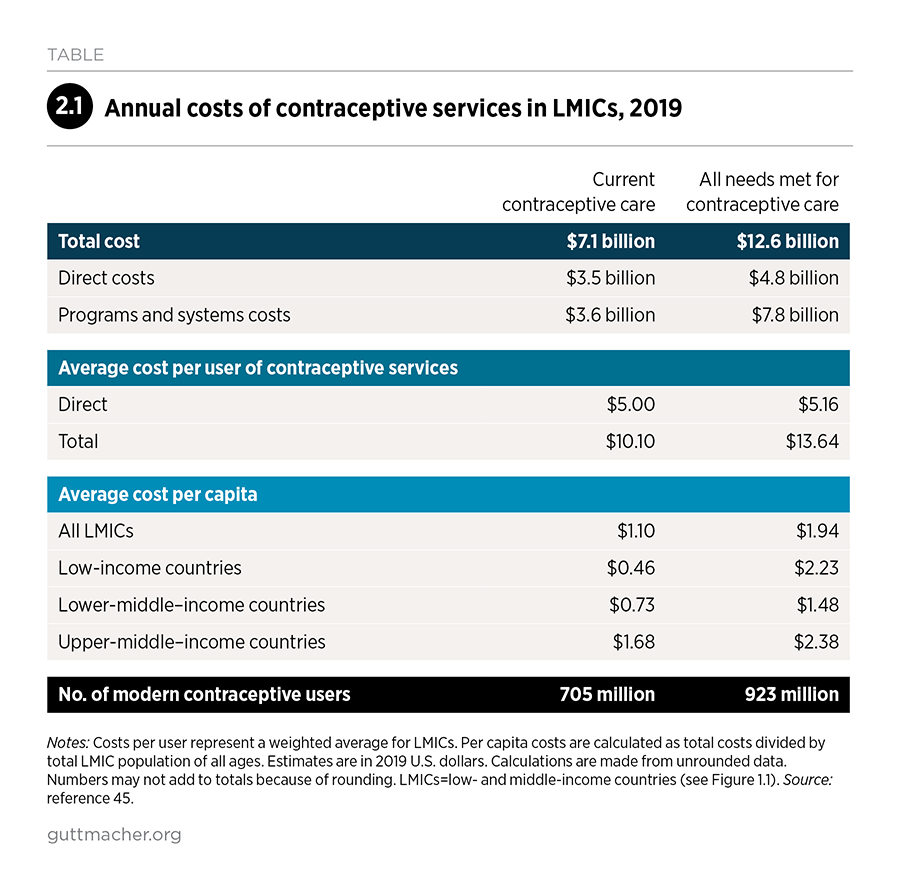
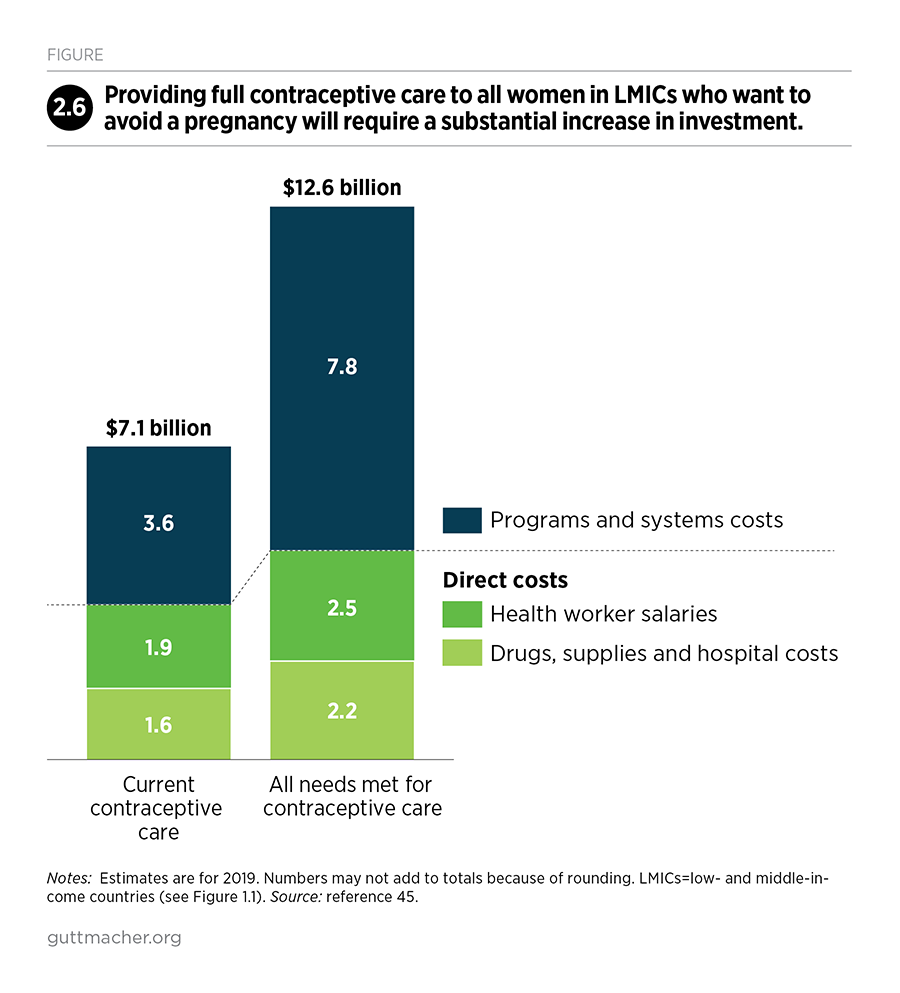
Current cost of contraceptive services
Based on estimates for 2019, the direct cost of contraceptive services for 705 million users in LMICs is $3.5 billion annually (Table 2.1).††45 Direct costs include contraceptive commodities, drugs, supplies and health worker salaries—all of which are required to provide clients with information and counseling, a range of methods, and removal services for implants and IUDs. In addition, the costs of the health programs and systems that underpin current contraceptive services are approximately $3.6 billion per year. These programs and systems costs include critical health systems elements, such as program management, staff supervision and training, infrastructure and equipment, and commodity and information management systems (see Box 1.1 for a complete list of components).
The average annual direct cost per user of modern contraceptives in LMICs is $5.00. This cost varies by method: Long-acting and permanent methods, such as IUDs and sterilization, cost more up front than short-acting methods do, but their costs are defrayed over a longer period of pregnancy protection. Thus, average annual direct costs per user are lowest for IUDs ($1.10), male sterilization ($1.33) and female sterilization ($2.10). Annual costs per user are substantially higher for short-acting hormonal methods‡‡ ($10.21) and male condoms ($6.65).
Costs also vary widely by region because of variations in method and personnel costs and the mix of methods used. The average cost per user is lowest in Asia ($3.77), where nearly three-quarters of current users live. This is primarily because permanent and long-acting methods are more commonly used in this region than in other regions (e.g., female sterilization is prevalent in India and IUDs are common in China). The average per-user cost is higher—$7.75 in Africa, $9.08 in Latin America and the Caribbean, $5.40 in Oceania and $6.48 in Eastern and Southern Europe—where the costs of the most-used contraceptives are higher.
The cost of meeting all women’s needs for contraceptive services
If the 218 million women with unmet need for modern contraceptives were to use the same mix of methods as current users of modern methods, direct costs would increase to $4.8 billion annually (Table 2.1).45 Programs and systems costs would increase to a greater extent, to $7.8 billion, bringing the total to $12.6 billion (Figure 2.6).
The cost increase associated with moving from current levels of contraceptive care to providing quality services to all women who need them mainly reflects the magnitude of the investments needed to expand programs and systems capacity and improve the quality of care. The improvements (and associated investments) needed are largest in the poorest countries, where health care systems are weakest and unmet need is highest. Investments in programs and systems will be essential for all women who need modern contraception, so they can make an informed choice about which methods to use, obtain counseling on how to use those methods effectively and receive continuous supplies as needed. These investments would also help remove barriers faced by economically disadvantaged communities and marginalized groups, such as young people and people living with disabilities or HIV/AIDS. Contraceptive services should be available to all people and free from discrimination and stigma.4
Areas in which improvements are needed include the following:
- Provision of accurate information and education
- Provision of a range of modern methods
- Logistics to ensure a continuous flow of supplies
- Availability and adequacy of service sites
- Trained health care workers, including community-based workers
- Availability and quality of counseling on methods and side effects
- Provision of follow-up services, including for removal of long-acting reversible contraceptives
- Outreach activities to increase awareness of the benefits of contraceptive services and to motivate individuals to use them
If all unmet need were satisfied, the direct cost per user would increase only slightly from $5.00 to $5.16 annually.45 These estimates assume that all women with unmet need would use modern contraceptives and that new users would use the same mix of methods as current modern method users in the same country of the same age, marital status and childbearing preferences. These assumptions are not meant to be prescriptive but rather to show the potential impact of scaling up services. If fewer women were to adopt a modern method, both the costs and impacts of services would be lower. If more women were to choose highly effective methods and were supported in using their methods more consistently and correctly, the impacts on unintended pregnancy would be greater than those presented here.61
The total costs of providing modern contraceptives to all 923 million women in LMICs who want to avoid a pregnancy amount to $1.94 per capita (i.e., per total LMIC population of all ages). Greater investment is needed in the poorest countries: The total in low-income countries would increase from $0.46 per capita for current care to $2.23 per capita to satisfy all needs. This investment to expand a proven, cost-effective health intervention62 for all women who need it would benefit women, their families and societies, and would help fulfill women’s sexual and reproductive rights.
3. Pregnancy-Related and Newborn Health Services
Worldwide, maternal and newborn deaths have declined dramatically over time, yet mortality levels remain unacceptably high in many low- and middle-income countries (LMICs).33,63,64 Because of stronger gains in the prevention of mortality among older children, newborn deaths account for an increasing share of all deaths among children younger than five (47% in 2018).64 The vast majority of maternal and newborn deaths occur in Sub-Saharan Africa and Southern Asia, where health systems are weak, too few health workers are trained and equipped to provide lifesaving care, and the quality of care provided is low.65–67 The impact of weak health care systems is compounded by broader factors such as poverty, poor nutrition, poor sanitation and exposure to communicable diseases.
A range of essential services is necessary to protect and enhance women’s health before, during and after pregnancy, and to give newborns a healthy start in life.68 All pregnancies and births pose some health risks to the pregnant woman and newborn. The World Health Organization (WHO) has established standards of care—during pregnancy, childbirth and after delivery—which this report uses to gauge the adequacy of care women and newborns receive and to estimate the costs of fulfilling unmet need for pregnancy-related and newborn care.69–71
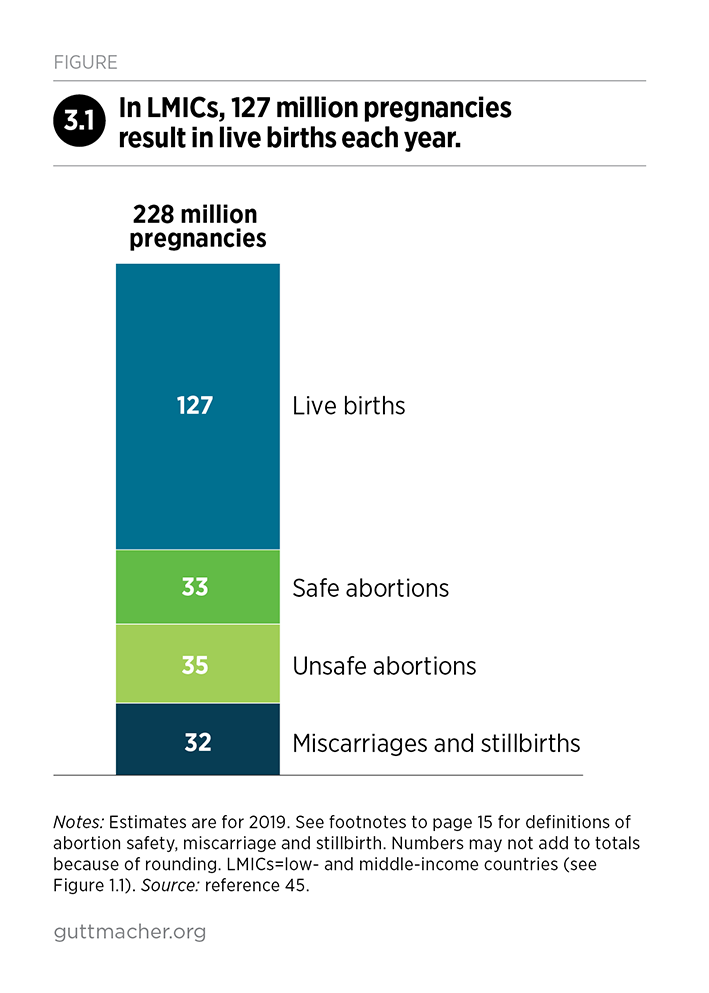
Out of 228 million pregnancies that occur in LMICs, an estimated 127 million—or 56%—result in a live birth each year (Figure 3.1).45 The other 101 million pregnancies result in abortions, miscarriages and stillbirths. All pregnant women should be able to get the essential care they need, regardless of the outcome of their pregnancy. Those who need more specialized medical services because of their individual risks or because of emergency situations should receive these services without delay.
The following health services for pregnant women and their newborns are covered in this chapter:
- Antenatal care with a skilled provider, including diagnosis and treatment of ectopic pregnancies
- Delivery in a health facility, including routine care for the mother and newborn
- Postnatal care for the mother and newborn, including routine checkups and support for breast-feeding
- Care for medical complications that arise during pregnancy, childbirth and shortly after birth for the woman and newborn
- HIV-related care for pregnant women and newborns, including prevention of mother-to-child transmission
- Safe abortion care and care for women experiencing complications after an unsafe abortion
Many specific actions are recommended within these categories, such as antenatal screening and treatment for preeclampsia, anemia and malaria; screening and treatment for infections such as syphilis, tetanus and tuberculosis; delivery care and active management of the third stage of labor; counseling about breast-feeding; and vaccinations and treatments for newborns.69,72,73 In total, our estimates cover more than 80 pregnancy-related and newborn health interventions (a complete list can be found in the methodology report at https://www.guttmacher.org/report/adding-it-up-investing-in-sexual-repr…).
Receipt of antenatal care
Good-quality antenatal care offers women the information, counseling and services they need to have a healthy pregnancy. Services include screening, preventive care and treatment for a range of conditions, such as hypertension, malaria, syphilis and anemia, that could jeopardize the health of the woman or her child. In this analysis, we consider women who have had four or more antenatal visits—at least one of which was with a skilled provider (midwife, nurse or doctor)—as having received the standard level of care. In 2016, WHO updated its minimum recommended level of care from four antenatal visits to eight contacts with the health system during pregnancy, including through community outreach;70,74 however, the available survey data are not sufficiently detailed to measure this updated standard of care.
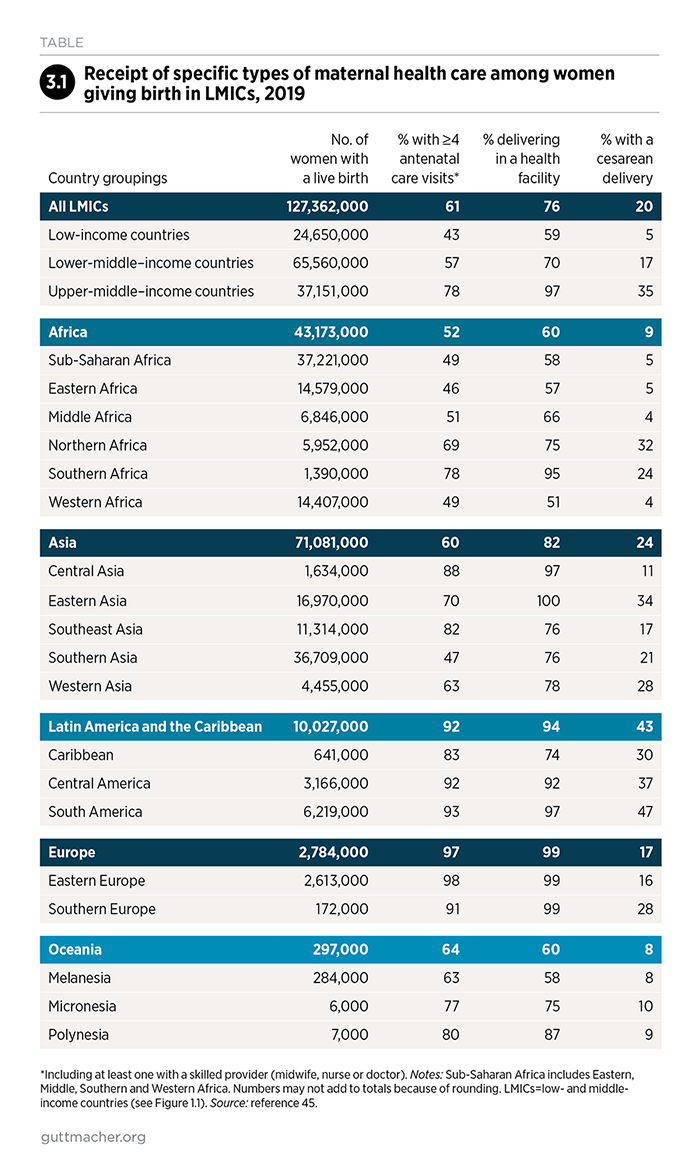
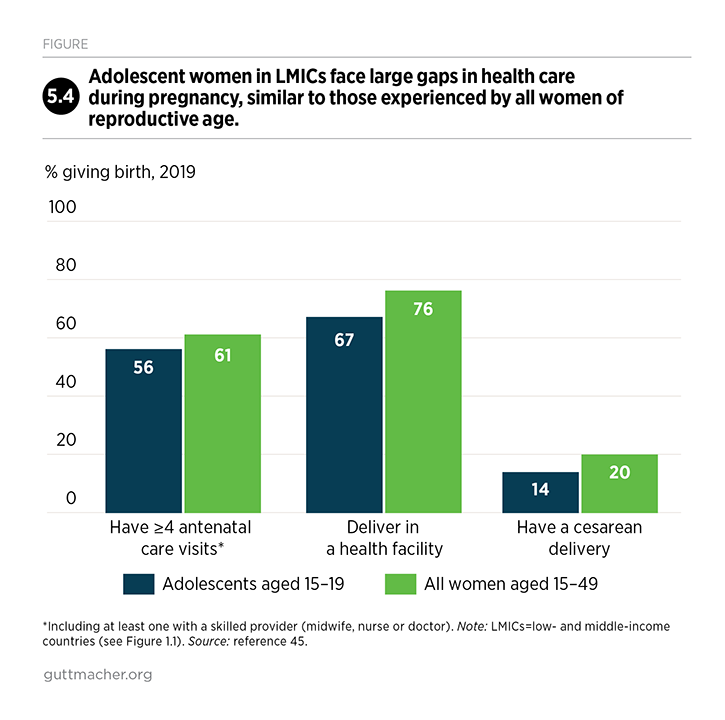
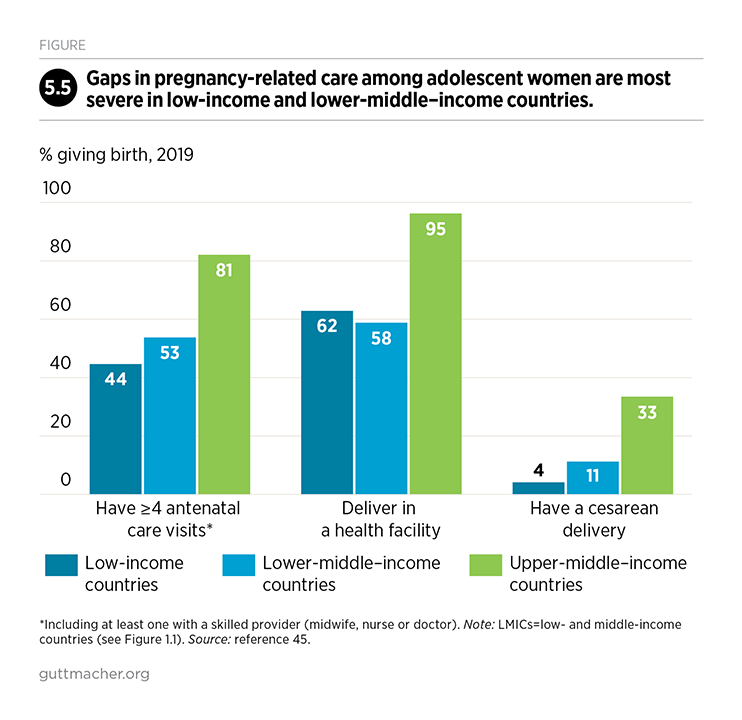
In LMICs, 61% of women giving birth make four or more antenatal visits (Table 3.1).45 In upper-middle–income countries, 78% receive this minimum level of care, compared with 57% of those in lower-middle–income countries and only 43% in low-income countries. There are also wide disparities by subregion: Fewer than half of women giving birth in Eastern Africa, Western Africa and Southern Asia make at least four antenatal visits, while more than 90% do in Central and South America and Eastern and Southern Europe. Also, the proportion receiving four or more antenatal care visits is relatively low among adolescents (56%; see Chapter 5 for more information on adolescents).
Even when women receive antenatal care, they do not necessarily receive all the essential components recommended by WHO. A recent study showed that across 10 LMICs covering all geographic regions, fewer than three-fifths of women making four or more antenatal care visits received all six essential routine services: blood pressure test, urine and blood tests, tetanus protection, iron supplementation and information on potential complications.75 Our analyses show that only 70% of women who get antenatal care receive a urine test as part of that care, with proportions ranging from 46% in low-income countries to 92% in upper-middle–income countries.45
Antenatal care should also provide pregnant women with screening and treatment (or a referral for treatment) for HIV and other STIs, but many women who need these services are not receiving them. (Testing and treatment for HIV and other STIs are essential services for all women of reproductive age and are discussed in Chapter 6.) If left untreated in pregnant women, curable STIs such as syphilis can lead to preterm labor, preterm delivery, low birth weight, congenital infection, and even stillbirth or newborn death.76 Untreated chlamydia and gonorrhea can also lead to serious health problems for women and newborns.41 Yet, antenatal screening practices for curable STIs vary around the world, by country and by particular STI.77
WHO’s current global strategy on STIs places priority on the elimination of congenital syphilis.78 The availability of a simple and rapid point-of-care syphilis test has made it possible for pregnant women to be tested and receive necessary treatment at the same visit.79,80 But greater efforts are needed to ensure all pregnant women receive this test as part of antenatal care. Currently, only 56% of women in LMICs receive the recommended screening for syphilis during their first antenatal care visit.45
Access to emergency medical care at delivery
Because the vast majority of maternal and newborn deaths occur around the time of delivery, skilled care at birth and access to emergency obstetric care are critical for saving women’s and newborns’ lives.81 While women and their babies benefit from having skilled assistance if they deliver at home, they need immediate access to treatment for delivery complications if they arise. Major complications of pregnancy or delivery—such as hemorrhage (severe bleeding), sepsis (infection), hypertensive disease (preeclampsia and eclampsia), or prolonged or obstructed labor—can lead to serious illness, injury and even death if not promptly and effectively managed. Women who deliver in a health facility have a better chance than those delivering at home to receive skilled care for routine deliveries and newborn care, as well as for obstetric complications, and to receive urgent care for their newborns, should such services be needed.
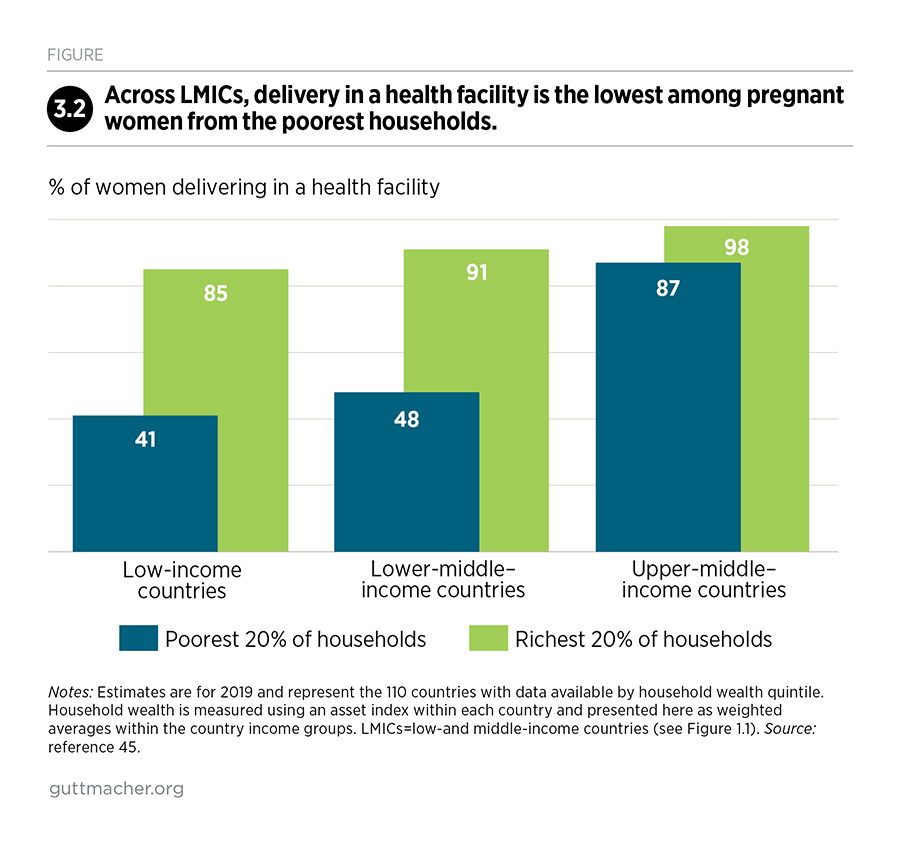
Across LMICs, about three-fourths of women deliver their babies in a health facility.45 This average masks large disparities across countries, however. The proportion of women delivering in a health facility ranges from 59% in low-income countries to 70% in lower-middle–income countries and 97% in upper-middle–income countries. Within countries, women’s receipt of maternal health care is strongly correlated with household wealth, and delivery in a health facility is lowest among the women from the poorest households (Figure 3.2).45 Inequalities are greatest in low- and lower-middle–income countries; the poorest women in the poorest countries face the greatest unmet need. The proportion of women with skilled assistance at birth—another indicator commonly used to measure progress toward reducing maternal deaths—follows a pattern similar to delivery in a health facility in most of the world (download the appendix tables above).
The proportion of women delivering in facilities has increased in every world region and across diverse settings in the last two decades.67 Yet, as of 2019, many women still do not receive needed care for major maternal complications. In LMICs, more than one in four women (27%) experience major complications during pregnancy, delivery or the immediate postpartum period, and 48% of these women do not receive the urgent medical care they need.45 Some women do not receive care because they do not deliver in a health facility; others deliver in a facility that does not provide the needed care. Barriers to providing and receiving effective care are described in more detail below (see Unmet need for pregnancy-related and newborn care).
Access to facility-based care gives women a better chance of receiving lifesaving procedures, such as a cesarean delivery. However, although this procedure can save the lives of women and their newborns, cesarean rates higher than 10% are not associated with reduced maternal and newborn mortality.82 Cesarean deliveries tend to be overused in higher income countries and underused in poorer countries.83 Cesarean rates are higher than 20% in Latin America and the Caribbean; Northern and Southern Africa; Eastern, Southern and Western Asia; and Southern Europe (Table 3.1).45 They are well below estimated levels of need in Eastern, Middle and Western Africa.
Postnatal care
Mothers and newborns also need postnatal care to address routine and emergency health needs in the hours and days after a birth.69 Postnatal care—measured here as a postnatal visit for the mother within 24 hours of delivery (including care received while still in the delivery facility)—is critical for managing hemorrhage and sepsis, which are the leading causes of maternal and newborn deaths, respectively, in LMICs.33,34 However, of all the interventions in the continuum of maternal and newborn care, postnatal care has some of the lowest coverage.45 As of 2019, an estimated 36% of new mothers in LMICs receive postnatal care.
Postnatal care should include counseling on birthspacing and contraception, and the provision of contraceptive methods on request.69 Extensive evidence from many years of surveys in LMICs supports the case for spacing births by at least two years. Overall, children born at shorter intervals face a higher risk of death, and the risk is even greater if the mother has had many children.84 Birthspacing is also good for mothers, as women who become pregnant less than six months after a birth are at increased risk of pregnancy complications and maternal death and disability.85 Postpartum contraceptive counseling and method provision are high-impact, effective interventions that can raise awareness of the benefits of birthspacing, reach women and their partners while at a health facility, and offer a range of contraceptives appropriate for postpartum women (see Box 4.2).86
Newborn care
About three-quarters of newborn deaths occur in the first week of life, and newborn deaths overall can be attributed to three main causes: sepsis, asphyxia (breathing difficulties) and complications related to preterm birth.34,87 Interventions included in a continuum of care that covers pregnancy, birth, the postnatal period and infancy could prevent many of these deaths. Some interventions take place during the mother’s antenatal care, such as screening and treatment for malaria, syphilis or hypertensive disease, and have a beneficial impact on newborns. Other interventions are focused on the newborn:71
- Provision of a clean delivery surface and hygienic cord care
- Resuscitation with a bag and mask for babies who are unable to breathe
- Drying the baby and keeping it warm
- Support for breast-feeding in the first hour after birth
- Special care for low-birth-weight and preterm babies (such as skin-to-skin contact for warmth)
- Treatment of local infections
In LMICs, 31% of newborns experience major complications, and among that group, 34% do not obtain the medical care they need.45 The proportions of women and newborns with unmet need for care for major complications are somewhat similar, since recognition and treatment of both sets of conditions are likely to happen only if a skilled professional is present.
Care for pregnant women living with HIV and their newborns
Women living with HIV who become pregnant need care, support and treatment for their own health and well-being, as well as to reduce the risk of transmitting the virus to their newborn. Antiretroviral therapy has greatly reduced new HIV infections among infants, although most countries with high levels of HIV infection fall short of providing all pregnant women living with HIV with lifelong antiretroviral therapy.88 Efforts must be increased to eliminate new infections among newborns altogether. One of the three areas of action in the Joint United Nations Programme on HIV/AIDS (UNAIDS) strategy to eliminate new HIV infections among infants and children is immediate treatment for all pregnant women living with HIV.
Our analysis looks at the need, impact and cost of HIV testing among pregnant women who do not already know they are HIV-positive, providing antiretroviral therapy for pregnant women living with HIV who are not already on treatment, and providing antiretroviral therapy to all newborns born to HIV-positive mothers.§§ See Chapter 6 for a broader discussion on HIV care.
Of the 127 million women with a live birth in LMICs as of 2019, an estimated 1.4 million are living with HIV.45 Most of these women (1.2 million) live in countries with generalized HIV epidemics (defined as an HIV prevalence greater than 1% among women with live births). Among these 1.2 million women, an estimated 81% receive antiretroviral therapy during pregnancy. In 2019, gaps in care—in countries both with and without a generalized HIV epidemic—resulted in an estimated 110,000 newborns in LMICs becoming infected with HIV during pregnancy or delivery.
Care for women whose pregnancies do not result in a live birth
In any given year, 101 million pregnancies in LMICs do not end in a live birth.45 Some 69 million end in abortions (35 million of which are unsafe), 30 million end in miscarriages and three million end in stillbirths (Figure 3.1). This translates into 44% of pregnant women annually who do not have a live birth: 30% who have an abortion, 13% who experience a miscarriage and 1% who have a stillbirth. These women have health care needs that existing services could address more effectively.
WHO recommends that all pregnant women receive antenatal care throughout the duration of their pregnancy, regardless of the pregnancy outcome.70 In addition, women with stillbirths should receive postpartum care, and women who decide to end their pregnancies should receive safe abortion services.
Survey data on the care received by women whose pregnancies do not result in a live birth are not available. Our analysis assumes that women who have stillbirths receive the same level of services as women in the same country who have live births, and that women who have miscarriages receive the same level of antenatal care as those giving birth, up to the time of pregnancy loss. Estimates of the costs of care for these women are included in the pregnancy-related care estimates presented in this chapter.
Abortion and postabortion care
For women undergoing an abortion, WHO generally recommends the least invasive abortion method appropriate to the stage of pregnancy.89,90 For most abortions, the guidelines recommend the use of vacuum aspiration or medication abortion (using a combination of mifepristone and misoprostol, or using misoprostol alone where mifepristone is not available). Dilation and evacuation is recommended in situations in which the other methods are contraindicated (typically in the second trimester). Abortions are defined as safe if they are offered by a trained provider using a recommended method.25
In this analysis, the proportion of abortions that are unsafe in a given country is based on 2010–2014 regional estimates (which have been adjusted to 2019) from WHO, the Guttmacher Institute and other authors, except where country-specific information is available*†25 The proportion of abortions occurring in 2010–2014 estimated to have been unsafe is extremely high (50% or more) in all regions of Africa except Southern Africa, all regions of Latin America and the Caribbean, and in a single combined region of Southern and Central Asia.
WHO provides standards of care for addressing postabortion complications,89 such as hemorrhage or infection, which most often occur where abortion is heavily restricted and unsafe. Contraceptive counseling and services are also recommended as essential components of both abortion and postabortion care.
Unmet need for pregnancy-related and newborn care
Despite progress in recent decades to make pregnancy and delivery safer, tens of millions of women in LMICs have an unmet need for maternal health care. Of the 127 million women who have a live birth each year, the following numbers of women experience gaps in essential services:45
- 50 million make fewer than four antenatal visits
- 31 million do not deliver their babies in a health facility
- 16 million need but do not receive care for major obstetric complications
- 13 million have newborns who need but do not receive care for major complications
In addition, women whose pregnancies do not result in a live birth also experience unmet needs for care:
- 35 million have abortions in unsafe conditions
- 9 million do not receive the necessary care for complications after an unsafe abortion
- 2 million do not receive needed treatment after a miscarriage
Why do so many women lack essential care during pregnancy and delivery? Much of the unmet need reflects lack of access to and poor quality of pregnancy-related and newborn care, which in turn, is often due to weak and underfunded health systems.67,91–94 Some facilities are not equipped to provide the necessary care because they have too few trained providers, or because the necessary lifesaving drugs and supplies are not available. Also, lower-level facilities may fail to transport women promptly to higher-level facilities that can provide the necessary care. In addition, some women may not recognize they are experiencing a complication that requires medical attention or they may lack transport to a health facility.
Other evidence suggests that some providers’ discriminatory attitudes and abusive behaviors may deter women from obtaining the care they need.95–98 For example, women who go to facilities to give birth may encounter disrespect or verbal or physical abuse. They may also receive care that lacks dignity, confidentiality or informed consent. These problems are systemic and persist for many reasons: Some providers may be overworked and stressed or may believe they should be in control of their patients, staff supervision may be weak and accountability mechanisms lacking, and the facilities may not have a culture of respecting women.
Women seeking abortion services face particularly harsh conditions—the barriers mentioned above, as well as legal restrictions and other operational barriers, such as medical guidelines that restrict access. In the large majority of LMICs, most women, especially those who are poor, do not have access to safe and affordable abortion services. Even in countries where the procedure is legally permitted under some circumstances, women often face considerable obstacles to obtaining legal and safe services, including lack of information about the process for getting a safe procedure, inability to pay, social stigma, a shortage of trained providers and providers’ unwillingness to offer the services.99
As is discussed in Box 2.2 with regard to contraceptive care, providing quality pregnancy and delivery care in a way that protects people’s human rights would address many of these issues.100 Solutions include using evidence-based approaches to care, improving training for health professionals, and making greater use of midwives and community health workers,101 who, with the necessary training, can provide referrals and effective services. Finally, moving toward universal health coverage could help to improve access to care where it is currently unaffordable.
Health impacts of pregnancy-related and newborn care
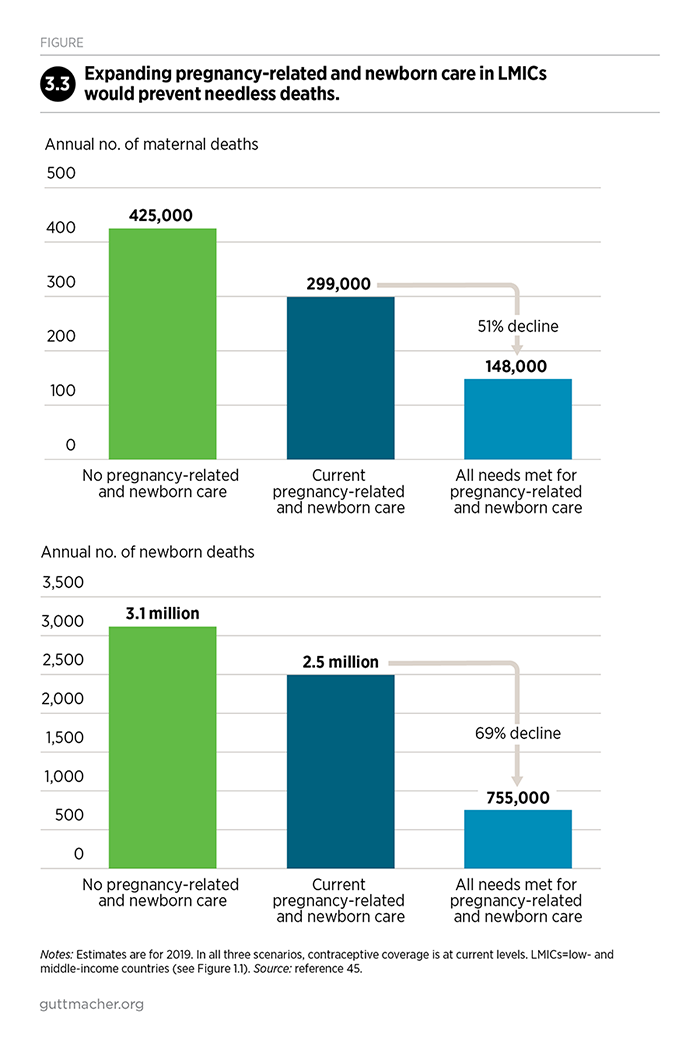
The current level of pregnancy-related and newborn care—for women who have live births, as well as those who have abortions, miscarriages or stillbirths—prevents at least 126,000 maternal deaths per year. Therefore, the total number of deaths that would occur in the absence of such services (at least 425,000) is reduced to 299,000 per year (Figure 3.3).45
Providing all pregnant women and newborns with the recommended care would reduce the burden of death and disability even further. By lowering the risk of complications and providing immediate care for those who experience complications, expanded care that meets WHO standards would have the following impacts on maternal and newborn health:
- A 51% decline in maternal deaths, from 299,000 to 148,000
- A 69% decline in newborn deaths, from 2.5 million to 755,000
- An 88% decline in new HIV infections among newborns (within the first six weeks of life), from 110,000 to 14,000 (data not shown)
Costs of expanding and improving care
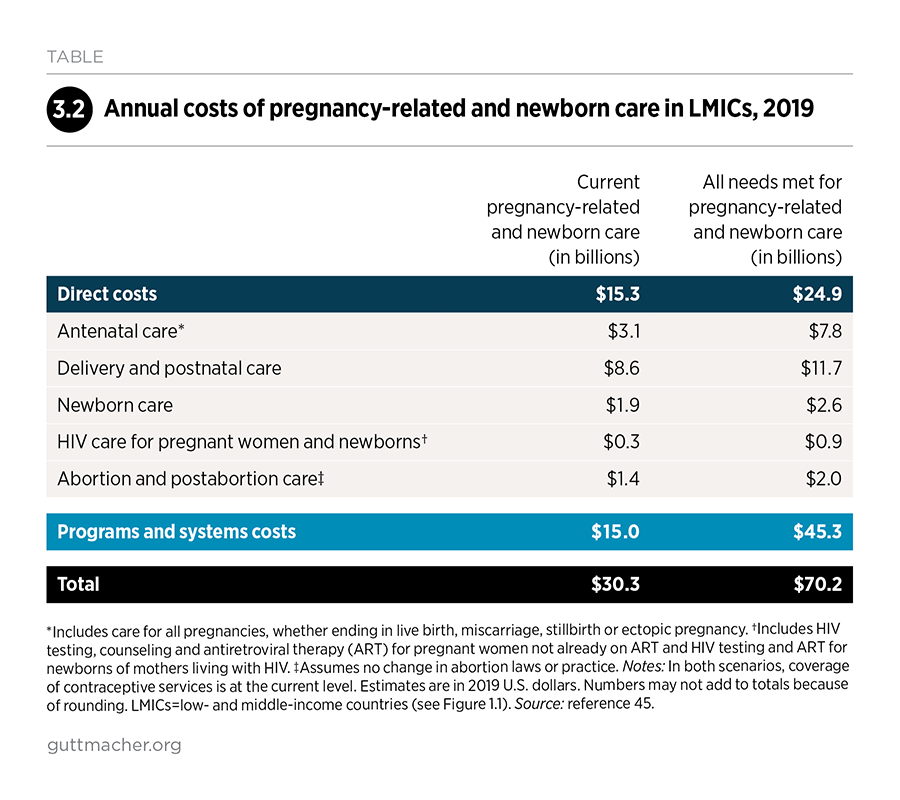
The direct cost of providing pregnancy-related and newborn care at current levels of coverage is estimated at $15.3 billion for 2019 (Table 3.2).45 Delivery and postnatal care account for the largest share of the total direct cost (56%, or $8.6 billion), followed by antenatal care and newborn care. Abortion and postabortion care and HIV-related care for newly diagnosed pregnant women and the newborns of all women living with HIV account for smaller shares of costs.
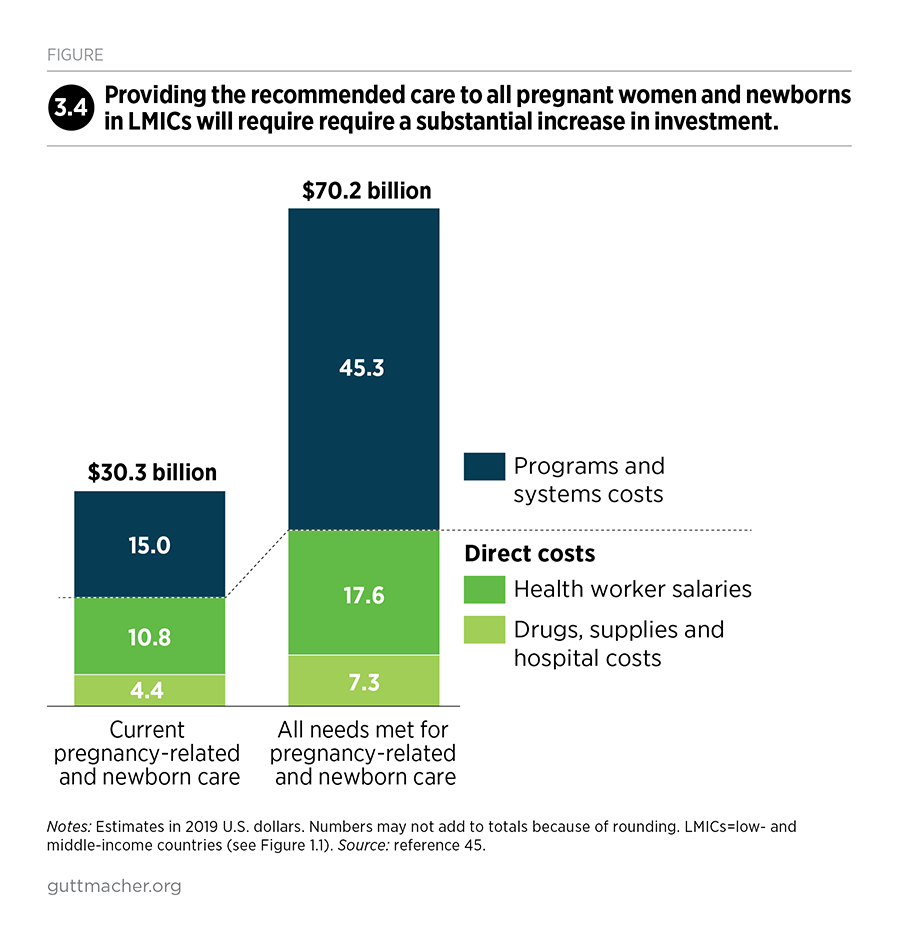
To provide the recommended pregnancy-related and newborn care to all who need it, direct costs would increase to $24.9 billion per year. This estimate is based on numbers of pregnancies at current levels of contraceptive use.
Personnel costs are the largest component of direct costs. At current levels of coverage, health worker salaries account for 71% of direct costs, while medications, diagnostic tests, supplies and food costs (for inpatient hospital stays) account for the other 29%. To attain full coverage of the recommended pregnancy-related and newborn care, personnel costs would increase from $10.8 billion to $17.6 billion per year, and other direct costs would increase from $4.4 billion to $7.3 billion (Figure 3.4).
Programs and systems costs for the current level of pregnancy-related and newborn care are an estimated $15.0 billion, bringing total current costs to $30.3 billion. For the scenario in which all pregnant women and newborns receive the recommended care, programs and systems costs would increase to $45.5 billion, and annual total costs would be $70.4 billion.
4. Combined Investment in Contraceptive Services and Essential Care for Pregnant Women and Newborns
Contraception and pregnancy-related and newborn care are interconnected parts of a continuum of essential care that supports women’s health throughout their reproductive lives and protects their children’s health.4 Simultaneous investment in both sets of services would generate greater benefits than investing in either one alone—and it would produce cost savings. By preventing unintended pregnancies, improved contraceptive care would both avert maternal deaths and reduce costs associated with providing pregnancy-related and newborn care. Likewise, investment in safe abortion care would reduce the number of abortion complications, saving lives and reducing the cost of postabortion care.
Investing in contraceptive care alone would avert 70,000 maternal deaths each year (as shown in Chapter 2), and investing in pregnancy-related care alone would avert 151,000 maternal deaths per year (Chapter 3).45 But by jointly investing in contraceptive and pregnancy-related care, 186,000 maternal deaths would be averted. This represents a decline of 62% (from 299,000 to 113,000 per year), compared with smaller declines expected from an investment in contraceptive or pregnancy-related care alone (Figure 4.1). Moreover, the benefits of a joint investment extend well beyond health (Box 4.1).
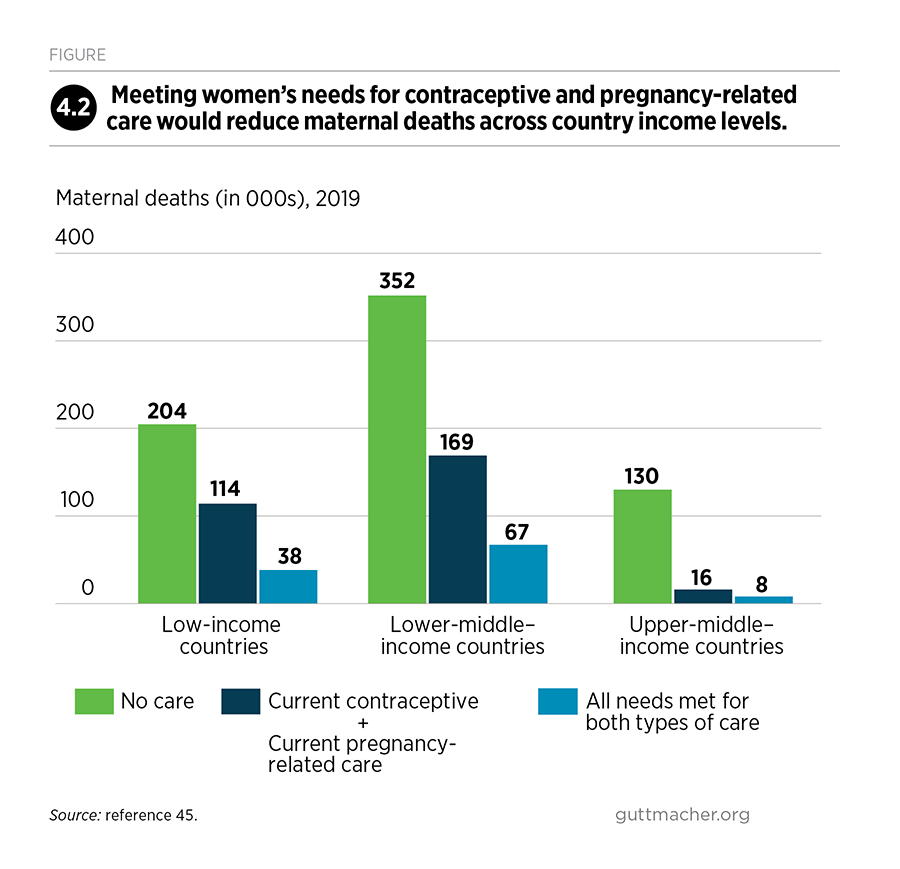
The additional investments would especially benefit low- and lower-middle–income countries. Current investments in contraceptive and pregnancy-related care avert 375,000 maternal deaths in LMICs, and most of these deaths are averted in lower-middle–income countries (Figure 4.2). Fully meeting the needs for contraceptive and pregnancy-related care would avert an additional 186,000 maternal deaths. Most of this benefit would accrue in low-income and lower-middle–income countries, where reductions in maternal deaths would total 76,000 and 102,000, respectively.
Box 4.1
Broader benefits of sexual and reproductive health care
Improvements in the sexual and reproductive health services analyzed in this report would result in many wide-reaching benefits beyond the health impacts quantified here. These include improvements in gender equality, economic well-being for women and households, productivity, resources for children and gross domestic product (GDP), as well as reduced harm to the environment. While these and other broad benefits are harder than health outcomes to quantify, studies indicate that the gains for individuals, families and societies are substantial.43,44,102,103
Social and economic benefits
Studies have drawn on various data and analytical approaches to show the broad social and economic benefits from investments in contraceptive and pregnancy-related and newborn care. One study of 74 countries with high maternal and child mortality found that increasing expenditures for reproductive, maternal, newborn and child health services by just $5 per capita per year to the year 2035 could yield up to nine times that value in economic and social benefits, including greater GDP growth through increased productivity.42 Evidence from experimental studies in the resource-poor areas of Matlab, Bangladesh, and Navrongo, Ghana, where community-based family planning and health programs were introduced, showed that fertility declines were associated with improvements in women’s health, earnings and participation in paid employment.43 In addition, the children of women in areas with family planning outreach programs were healthier and better educated than children in other areas.
The demographic dividend
Some studies have shown that contraceptive use can contribute to a "demographic dividend"—accelerated economic growth resulting, in part, from a decline in a country's fertility and the subsequent change in the age structure of the population.104–106 With fewer births each year, the size of a country's dependent population grows smaller relative to the working-age population. In theory, with fewer younger and older people for workers to support, a country has a window of opportunity for rapid economic growth and a boost in per capita income. Thus, the dividend could be especially beneficial for emerging economies with younger populations. However, achieving the dividend is not a given. The right social and economic policies must be in place to provide education and employment opportunities for all people.
Benefits for the environment
Many experts view universal access to voluntary family planning as a "climate-compatible" development strategy.107,108 Reductions in unintended pregnancy through contraceptive use and women’s empowerment can help slow population growth, which in turn reduces demands on the environment. In addition, by influencing both the size and overall health of future populations, improved sexual and reproductive health care has a positive effect on households’, communities’ and countries’ ability to adapt and respond to environmental change.109,110
Cost savings resulting from a combined investment
As shown in Chapter 2, if all 218 million women with an unmet need for modern contraception were to receive care and services overall were improved, the total cost of contraceptive services would increase from $7.1 billion to $12.6 billion annually.45 The increased spending would result in 76 million fewer unintended pregnancies and 21 million fewer unplanned births in LMICs.
The reduction in unintended pregnancies would make improvements in pregnancy-related and newborn care more affordable. Providing health care for women with unintended pregnancies (whether the pregnancy ends in live birth, miscarriage, stillbirth or abortion), as well as for their newborns, currently costs $10.0 billion annually (Figure 4.3). But some pregnant women and newborns who need care do not receive it, and others receive inadequate care. If all women with unintended pregnancies and their newborns were to receive the recommended care, the cost of care for unintended pregnancies would increase to $22.9 billion. However, if all women wanting to avoid a pregnancy used modern contraception, the cost of pregnancy-related care for unintended pregnancies would decline to $6.6 billion.
In other words, investments in contraceptive services help offset the cost of improving pregnancy-related and newborn care for all women and their newborns. Keeping contraceptive care at current levels, while fully meeting the health care needs of pregnant women and their newborns, would cost $77.4 billion in LMICs. By comparison, fully meeting the needs for both contraceptive care and pregnancy-related and newborn care simultaneously would provide greater health benefits at a lower cost of $66.6 billion.
The health impacts and costs of abortion-related care
The current total cost of abortion-related care in LMICs is an estimated $2.8 billion annually, which includes $1.0 billion for abortions (provided under both safe and unsafe conditions) and $1.7 billion for postabortion care (Figure 4.4).45 These totals are included in the costs for pregnancy-related care shown in Figure 4.3.
Almost all postabortion care is for treating complications from unsafe abortion. Although abortion complications in LMICs account for only 6% of the current $30.3 billion cost of pregnancy and newborn care, they cause an estimated 8% of maternal deaths.45 These deaths reflect the poor conditions women face when obtaining unsafe abortions and the lack of effective services for those who experience complications requiring medical care.99
If women’s contraceptive needs were fully met in LMICs, the reduction in unintended pregnancies would result in large declines in abortions, especially unsafe abortions.45 The health complications resulting annually from unsafe abortions would drop dramatically, even if there were no change in the conditions under which abortions occur:
- A 62% decline in safe abortions, from 33 million to 13 million
- A 72% decline in unsafe abortions, from 35 million to 10 million
- A 74% decline in the number of women needing medical care for complications from unsafe abortion, from 20 million to five million
- A 78% decline in maternal deaths due to unsafe abortion, from 23,000 to 5,000
The declines in unintended pregnancies and unsafe abortions would reduce the cost of abortion-related care for all women needing abortion services from $2.8 billion to $1.5 billion.45
Even with full coverage of contraceptive and abortion-related care, 10 million unsafe abortions would still occur—both because unintended pregnancies would not be eliminated entirely and because restrictive laws and barriers mean that many women in LMICs who want to terminate an unintended pregnancy must resort to unsafe abortion. These remaining unsafe abortions would require $1.0 billion for postabortion care. Postabortion care provides necessary, and sometimes urgent, care for women experiencing complications from unsafe abortions, as well as contraceptive counseling and effective contraceptive methods to prevent future unintended pregnancies (Box 4.2).
Expanding women’s access to safe abortion services would further reduce maternal deaths in LMICs. In addition, these investments would dramatically reduce the cost of postabortion care. If all abortions in LMICs that are currently unsafe were provided safely, and if all needs for contraceptive and abortion-related care were met, the total cost of abortion-related care for women needing abortion services would decrease to $0.6 billion.
Box 4.2
Integrating contraceptive services with postpartum and postabortion care
A key juncture for contraceptive counseling and provision of methods is after a birth or an abortion. Studies have shown significant unmet need for contraception among postpartum women. Meeting the need is complicated, however, because many women worry that contraception will interfere with breast-feeding.111 Counseling—which would include informing women that many modern methods can be used safely and effectively while breast-feeding—can begin during antenatal care to give adequate time for discussing women’s options and preferences. But counseling only once during antenatal care has not proven sufficient for increasing postpartum contraceptive use; antenatal and postpartum counseling combined has shown better results.111 Counseling women and providing them with a method after they give birth but before they are discharged from a health facility may be the optimal intervention in places where many women do not return for postnatal health visits. Providers must ensure that women understand their options, can make informed choices and choose a method voluntarily.112 Contraceptive counseling and services can also be integrated into other types of health care visits, such as visits for infant immunization.
For women who have had an abortion, the ability to conceive usually returns within a few weeks,113 and according to World Health Organization guidelines, women may initiate contraceptive use immediately after surgical or medication abortion.90,114 The guidelines recommend that postabortion care include offering the full range of methods, including the most effective reversible methods (IUDs, implants and injectables), which can be provided onsite before a woman leaves a health facility.115 However, data from LMICs show major weaknesses in postabortion contraceptive provision.111 In many settings, women do not receive contraceptive counseling after an abortion, and reasons include lack of trained staff, heavy workloads among providers, stockouts of methods and providers’ lack of knowledge about how long it takes for fertility to return.93,99,116,117
5. Contraceptive, Pregnancy-Related and Newborn Care for Adolescents
Adolescence, the period in which young people transition from childhood to adulthood, is a critical time to invest in sexual and reproductive health. In LMICs, many young women become sexually active, marry and start childbearing between the ages of 15 and 19, often without the support of policies and programs that would enable them to make informed and voluntary decisions to protect their health and exercise their sexual and reproductive rights.4,118
International commitments regarding adolescent sexual and reproductive health emphasize both the unique challenges that people face at this point in the life course, as well as the longer-term benefits of investing in effective services for adolescents.3,119 In addition, the 2030 Agenda for Sustainable Development explicitly aims for a world in which the voices of the most vulnerable are heard and the needs of the most vulnerable are met.1 Adolescents are among the most vulnerable groups with respect to their sexual and reproductive health–related needs and their ability to have their voices heard on matters related to their sexuality.120 Contraceptive, pregnancy-related and newborn health information and services are among a wide range of interventions necessary to fully support adolescents’ health and rights.121
An estimated 261 million women aged 15–19 live in LMICs as of 2019.45 These adolescent women represent 16% of women of reproductive age (15–49) in LMICs. They represent 22% of reproductive-age women in low-income countries, where recent high rates of population growth have meant that adolescents make up a disproportionate share of the population. By 2030, the number of adolescent women aged 15–19 in LMICs overall will increase to 286 million.6
This chapter presents data on contraceptive and pregnancy-related and newborn health services for adolescent women in LMICs. We present the need for and use of services for which we have age-specific data, either from country surveys or model-based estimates. For other estimates (e.g., the cost of services), the underlying data are not age-specific but are based on rates or costs pertaining to all women of reproductive age. The need for and cost of STI treatment (discussed in Chapter 6) also pertains to all women of reproductive age.
The groups of adolescents for whom information is limited, and whose needs are often overlooked, include adolescents younger than 15,122,123 adolescents with disabilities, racial and ethnic minorities, indigenous populations and LGBTQ adolescents. We use the term "adolescent women" to match the data available in nationally representative household surveys, although we recognize that not all people have binary gender identities.
Context of sexual activity and unintended pregnancy
Studies show that in all regions globally, the age at which adolescents begin sexual activity has changed little over time, while the ages of marriage and first birth have risen substantially.121 Still, for many adolescent women in LMICs, sexual activity occurs within a marital or cohabiting union. About one in five (21%) young women marry before age 18,124 the internationally recognized age of adulthood.125 Levels of child marriage are particularly high in Southern Asia (30%), Eastern and Southern Africa (35%) and Western and Central Africa (41%).124 This harmful practice often means adolescent women and younger girls have little say in choosing whom or when they will marry and have little power within the marriage to protect their sexual and reproductive health.118
In nearly every country with available data, some adolescent women aged 15–19 are sexually active outside of marriage. In general, levels of unmarried adolescents’ sexual activity are higher in Africa and Latin America and the Caribbean than in Asia, but the levels in Asia are likely to be underestimated.46 In Asia, as well as in Northern Africa, never-married women are often excluded from fertility and health surveys. Moreover, when people are asked about sexual activity in a face-to-face survey interview (a key source of data for these estimates), they tend to underreport it.126
Regardless of their marital status, adolescents have the right to decide whether to be sexually active, to engage in consensual sexual relations and to have their bodily integrity respected.4 Too often, though, the context of adolescent sexuality violates these rights. For example, the World Health Organization (WHO) estimated in 2013 that 29% of ever-partnered 15–19-year-old women worldwide had experienced intimate partner violence.127
As of 2019, adolescent women aged 15–19 in LMICs have an estimated 21 million pregnancies each year.45 One half of pregnancies are unintended, and 55% of unintended pregnancies end in abortions, which are often unsafe. These numbers reveal this age-group’s large unmet need for contraceptives and safe abortion care.
Contraceptive use and unmet need
Of the 261 million adolescent women aged 15–19 in LMICs, 88% (229 million) are not at risk of unintended pregnancy and do not currently need contraceptives, mainly because they are unmarried and report not having had sexual intercourse in the last 30 days (Figure 5.1).*‡45 Others do not need contraceptives because they want a child in the next two years, are pregnant or postpartum with an intended pregnancy, or are not able to become pregnant.
Twelve percent of women aged 15–19 in LMICs—32 million adolescent women—need contraceptives because they are currently sexually active, either within or outside of marriage, and do not want a child for at least two years. Of the adolescent women in need, 57% (18 million women) are using a modern method. The other 43%, or 14 million women, have an unmet need for modern contraception. Adolescent women account for 6% of all women of reproductive age with an unmet need for modern methods.
Among women who want to avoid a pregnancy, adolescents have a higher unmet need for modern contraception than do all women of reproductive age (43% versus 24%; Figure 5.2). The age disparity in modern method use is larger than disparities by rural-urban residence or socioeconomic status.49 In addition, adolescents living in low- and lower-middle–income countries have proportionally greater unmet need for modern methods, compared with adolescents living in upper-middle–income countries (Figure 5.3).45
The large majority of adolescent women with an unmet need for modern methods are using no method at all (85%), while the rest rely on a traditional method (15%). Among adolescents using modern contraceptives, almost nine out of 10 are using short-acting methods (most commonly condoms, pills and injectables). Relatively few adolescent women use long-acting reversible methods (implants and IUDs), and sterilization is rare.
Context of adolescents’ contraceptive choices
Adolescents’ contraceptive use is uniquely shaped by numerous social, cultural and economic circumstances.128 Among adolescents who use a method, preventing unintended pregnancy is typically a primary motivation, and some may also use contraceptives to prevent transmission of HIV and other STIs, and to have control over their own body, more generally. Other adolescents who want to avoid becoming pregnant may be reluctant or unable to obtain and use contraceptives—for instance, because they are unmarried and fear exposing that they are sexually active, because they are married and feel social pressure to have a birth, or because providers deny them appropriate care.
An analysis of unmet need in developing countries found that women of all ages who are not using contraceptives despite not wanting a pregnancy generally cite similar reasons for nonuse.52 For example, they often choose not to use a method because they have concerns about side effects or because they are postpartum and breast-feeding. The reasons most commonly cited by unmarried women are that they have sex infrequently and that they are not married. They may be concerned that seeking or using a contraceptive method would call attention to behavior that is often socially stigmatized, or they may underestimate their likelihood of becoming pregnant if they only occasionally have sex or if they have recently given birth.
Therefore, increasing awareness of the benefits of contraceptive services and building the capacity of adolescents to make their own decisions about using contraceptives is vital.128 Interventions with supporting evidence include combining educational programs in schools and communities with youth-friendly services, health center outreach activities and media campaigns.129 Activities that integrate improvements in service quality with efforts to generate community support for adolescent sexual and reproductive health are effective at increasing uptake of sexual and reproductive health services.130
On the services side, numerous program reviews have documented obstacles many adolescents face, such as judgmental attitudes of providers, lack of confidentiality, limited contraceptive options, and insufficient policies and guidelines for protecting adolescents’ rights to information and services.128,131 In terms of formal policies, nearly one in five countries worldwide have restrictions on access to contraceptive services: Requirements of parental consent for minors to receive services are among the most common restrictions and are in effect in 9% of the 186 countries with available data; restrictions based on a minimum age or marital status are in effect in 5% of countries.132 Even when countries do not have formal restrictions, however, adolescents face provider bias in various forms. Providers may not recommend hormonal methods to young people because of unfounded fears that the methods hamper a return to fertility, or providers may discriminate against unmarried young people out of a belief that they should not be sexually active.53 Recent recommendations on self-care interventions, such as self-administered injectables and over-the-counter oral contraceptive pills,133 could help adolescents overcome some of these systemic barriers.
Pregnancy-related and newborn care
Pregnant adolescents need the same high-quality maternal and newborn care, and abortion and postabortion care as all other pregnant women. As described in Chapter 3, WHO recommendations call for professional antenatal care visits with adequate screening for medical conditions (including HIV and syphilis), safe delivery care in a health facility, immediate care for obstetric complications, essential newborn care, and care for pregnancies that end in abortions, miscarriages and stillbirths. The proportion of adolescents receiving these types of care are described below for the services for which age-specific data are available.
Antenatal care. On average in LMICs, barely more than half (56%) of adolescents who give birth receive four or more antenatal care visits; similarly large gaps in this service are faced by pregnant women of reproductive age overall (61%; Figure 5.4).45 Only 44% of adolescents who give birth in low-income countries meet this standard, compared with 53% of those in lower-middle–income countries and 81% in upper-middle–income countries (Figure 5.5). Care also varies across subregions: No more than half of adolescents who give birth in Eastern, Middle and Western Africa and in Eastern and Southern Asia make the recommended minimum number of visits, while 90% or more do in Central America, South America and Eastern Europe. (Subregional differences are shown in the appendix tables, which can be downloaded above.)
Delivery in a health facility. Two-thirds (67%) of adolescents in LMICs deliver their babies in a health facility.45 This proportion varies widely across countries, from 58% in lower-middle–income countries to 95% in upper-middle–income countries. Other research shows that in Sub-Saharan Africa, adolescent first-time mothers are less likely than older first-time mothers to deliver at a health facility.134
Cesarean delivery. Cesarean deliveries represent 14% of all adolescent women’s deliveries, and levels vary sharply by country income group.45 In low-income countries, only 4% of adolescents have cesarean deliveries, compared with 33% in upper-middle–income countries. Rates lower than 10% tend to represent underuse of this lifesaving technique, while rates higher than 10% of deliveries are not associated with reductions in maternal and newborn mortality.82
Impacts of meeting adolescents’ needs
Adolescents in LMICs have an estimated 21 million pregnancies each year, 50% of which are unintended.45 Most of these unintended pregnancies (77%) occur among the 14 million adolescents who want to avoid a pregnancy but are not using a modern method (i.e., those with an unmet need for modern contraception). Another 22% of unintended pregnancies occur among those using short-acting methods, such as pills, condoms and injectables. Almost no unintended pregnancies occur among the relatively few adolescents who use long-acting reversible contraceptives, which have very low failure rates.35
At its current level, modern contraceptive use among adolescents in LMICs has a substantial positive impact. As of 2019, an estimated 18 million women aged 15–19 use modern contraceptives, thereby preventing 10 million unintended pregnancies that would occur if these adolescents used no modern methods (see Box 1.1 for a short description of how impact estimates were generated).45
Providing modern contraception to a larger proportion of adolescents who want to avoid pregnancy and improving the quality of contraceptive services overall would prevent additional unintended pregnancies, thereby improving young women’s health and lives, as well as those of their children. If adolescent women’s contraceptive needs were fully met, unintended pregnancies among women aged 15–19 in LMICs would decrease by 60%, from 10 million to four million per year (Figure 5.6). (Some contraceptive users—mostly those using condoms, pills and other methods that depend on users’ actions—would still have unintended pregnancies because of contraceptive failure.) Compared with current levels of contraceptive use, unplanned births would drop by 63%, from three million to one million per year; and abortions, most of which are likely to be unsafe, would drop by 58%, from six million to two million per year. These dramatic numbers represent gains forgone if inadequate levels of contraceptive care are allowed to persist.
An estimated 27,000 adolescent women per year in LMICs die from complications of pregnancy (including unsafe abortion) or childbirth, according to 2019 data.45 Current levels of pregnancy-related care prevent 10,000 additional deaths that would occur in the absence of such services.
Providing all pregnant adolescents with the recommended pregnancy-related care (for those who have live births, as well as those having abortions, miscarriages and stillbirths) would reduce deaths further, by reducing adolescent women’s risk of life-threatening complications and providing immediate care for those who need it. If all pregnant adolescents were to receive the recommended standards of care, adolescent maternal deaths in LMICs would drop by 54%, from the current level of 27,000 to 12,000 per year.45 If, in addition, adolescents’ need for modern contraceptives were fully met, the resulting drop in unintended pregnancies would reduce the need for pregnancy-related care. Thus, investing simultaneously in contraceptive services and pregnancy-related health care would have a greater health impact than investing in pregnancy-related health care alone: Adolescent maternal deaths would drop by 63% from the current level to 10,000 per year.
Cost savings resulting from a combined investment
Contraceptive services and pregnancy-related and newborn care for adolescent women and their newborns currently cost an estimated $0.42 per capita (i.e., per total population) per year in LMICs (Figure 5.7).45 If the recommended pregnancy-related and newborn care were provided to all pregnant adolescents and their newborns who needed it but contraceptive care remained at the current level, the combined cost of both sets of services would increase to $1.20 per capita. However, if all adolescents wanting to avoid a pregnancy were to use modern contraceptives, the cost of covering the two sets of services would be only $1.01 per capita. In a scenario in which investments are made in both sets of services simultaneously, each additional dollar spent on contraceptive services above the current level would reduce the cost of pregnancy-related and newborn care by $3.70.
Benefits beyond health
Investing in sexual and reproductive health services for adolescents, who are at a critical point in their lives, has far-reaching effects.135,136 The 2016 Lancet Commission on Adolescent Health and Wellbeing recommended increasing investments in young people to yield a "triple dividend of benefits": for adolescents now, for their future adult lives and for the next generation of children.121 A separate study supported this recommendation; it examined the benefits and costs of progressively scaling up interventions related to the health, education and well-being of adolescents to high levels of coverage by 2030.135 It found that a package of 66 health interventions—including services related to contraception, safe abortion and postabortion care, and HIV prevention and treatment—would cost $4.50 per capita per year when averaged across 40 LMICs for the period 2015–2030. The value of the economic and social benefits resulting from this large-scale investment in adolescents was estimated to be substantial, ranging from six to 17 times the costs of the interventions.
Along with interventions to end child marriage, the health investments could transform the lives of adolescent women by helping them avoid serious illness and death, prevent unintended pregnancies and unsafe abortion, reduce intimate partner violence, improve educational outcomes and provide young people access to better jobs.135 These investments would also enhance adolescents’ rights to bodily integrity and to pursue a satisfying, safe and pleasurable sexual life, free from stigma and discrimination. Although their benefits are difficult to measure, such rights are essential to human well-being and dignity.
6. Additional Sexual and Reproductive Health Services
As noted at the outset of this report, sexual and reproductive health services encompass much more than contraceptive services and pregnancy-related and newborn care. A quarter-century ago, the global community defined sexual and reproductive health care to include services addressing HIV and other STIs, gender-based violence, harmful practices such as female genital cutting, reproductive cancers and infertility, and sexual health and well-being.137 However, availability of and access to these services for women of reproductive age (15–49) in low- and middle-income countries (LMICs) have progressed in an uneven manner.
This chapter examines several sexual and reproductive health issues that have not been covered in previous chapters. We focus on those issues for which data are available on the magnitude of need and for which evidence-based interventions exist: the four major curable STIs, cervical cancer, HIV, intimate partner violence, infertility and the special concerns of people living in humanitarian crisis settings. Some important topics are excluded here, such as menstruation, menopause, and the sexual and reproductive health of people with disabilities and LGBTQ individuals. There is a critical need for additional documentation on these topics.
STIs
Globally, more than one million STIs are acquired every day, caused by bacteria, parasites and viruses.41 Each year, the four most common curable STIs—chlamydia, gonorrhea, syphilis and trichomoniasis—account for an estimated 376 million new infections among men and women worldwide.40 In addition, viral STIs, which are mostly incurable, affect hundreds of millions of people: More than 400 million people are living with genital herpes infection globally,138 and more than 290 million women have a human papillomavirus (HPV) infection.139 As of 2018, nearly 38 million people worldwide were living with HIV.140
The situation is particularly difficult for women and children. Many women with STIs experience few or no symptoms, and the infections can go undetected for years. When women do have symptoms, they may not seek care because of social stigma, poor access to care or other reasons. Yet, STI infections can compromise quality of life and lead to serious health problems for those affected.78 An estimated 40% of women with untreated gonorrhea or chlamydia infection develop pelvic inflammatory disease, which if left untreated, will lead to infertility in one in four cases.141 Mother-to-child transmission of syphilis can result in stillbirth, newborn death, low birth weight, prematurity and congenital deformities.142 Some STIs increase women’s risk of acquiring HIV threefold or more,41 and two specific types of HPV are responsible for most cervical cancer.143
This section focuses primarily on women’s need for and use of services for four major curable STIs. HPV, as it pertains to cervical cancer, is discussed in the following section, and HIV among women of reproductive age—including women’s need for care and treatment, and how living with HIV impacts other aspects of their sexual and reproductive health—is discussed later in this chapter.
New directions for STI testing and treatment in LMICs. Screening for STIs requires diagnostic tests and systems for case management. Historically, the diagnostic tests most widely used in high-income countries have been unavailable in many LMICs because the tests and laboratory infrastructure needed to process them are expensive. For low-resource settings, the World Health Organization (WHO) has long had guidelines for treatment of some STIs based on symptoms, but this approach, called syndromic management, misses the infections that do not have symptoms—which are the majority of STIs.41
In 2016, WHO released a strategy for a renewed global focus on the control of STIs.78 It calls for 70% of countries to have national surveillance systems and STI services integrated into primary care, maternal health and other sexual and reproductive health care by 2021. Achieving these goals will require scaling up existing screening programs and focusing on the populations most at risk, including individuals not experiencing symptoms, where feasible.
Fortunately, technological advances may help facilitate these ambitious improvements in care. Inexpensive and rapid blood testing to detect syphilis is already offered as part of antenatal care in many settings,79 and rapid dual HIV/syphilis kits allow for simultaneous testing.144 In recent years, similar tests have become available for other STIs, including chlamydia, gonorrhea, trichomoniasis, herpes and HPV. Although still too costly for many low-income countries, as uptake increases and the technology advances further, point-of-care testing will likely become more affordable.
Once diagnosed, the four major curable STIs can be treated with single doses of low-cost antibiotics (except in cases of drug-resistance, which has been identified in a small number of people with gonorrhea).145,146 By contrast, most viral STIs have no cure, though their symptoms can be managed. For some viral STIs (hepatitis B and HPV), vaccines now offer protection from infection.147
Curable STIs in women of reproductive age. In LMICs, roughly one in 10 women of reproductive age—an estimated 157 million women—contract one of the four major curable STIs each year (Table 6.1).45 The majority of these women (72%) do not have symptoms (Figure 6.1). Some asymptomatic infections—particularly of syphilis—may be caught by routine screening during pregnancy. However, routine screening for chlamydia, gonorrhea and trichomoniasis in pregnant women and other high-risk groups is not standard; as a result, few of these women will receive medical care for their asymptomatic infections. Among the estimated 28% of infected women who do have symptoms, about one-half (54%) receive medical care. Based on these estimates, about 24 million women (15% of those infected) obtain medical care, and approximately 133 million women (85% of those infected) have an unmet need for STI services.
As with other types of reproductive health care, whether a woman obtains care for an STI greatly depends on her economic status. In developing countries in 2014, about half of women aged 15–49 with an STI or STI symptoms obtained medical care, but the proportion obtaining care varied widely between women living in the poorest households (40%) and those living in the wealthiest households (65%).11
The low costs and substantial benefits of STI treatment. In LMICs, the current cost of treatment for women infected with any of the four curable STIs is an estimated $257 million, as of 2019, and this total includes both direct costs and programs and systems costs (Table 6.2).45 Given that very few asymptomatic women obtain care, this total includes treatment for only symptomatic women who receive care within the health system. The average cost per woman treated is $11, ranging from $5 in low-income countries to $14 in upper-middle–income countries (data not shown).
By contrast, treating all women in LMICs who are infected with any of the four major curable STIs—whether or not they have symptoms—would cost an estimated $2.3 billion annually. Antenatal care would cover a portion of this cost as part of meeting all needs for pregnancy-related and newborn health care. This is because WHO recommends screening and treating all pregnant women for syphilis80 and for symptomatic chlamydia and gonorrhea (to prevent newborn conjunctivitis).148 The total cost of treating these infections in pregnant women (all of which is included in the cost estimate for pregnancy-related and newborn care in Chapter 3) is $116 million.45
Treatment of chlamydia and gonorrhea among women at current levels prevents three million cases of pelvic inflammatory disease, which in turn prevents one million women from developing infertility from these infections each year.45 However, an estimated 30 million cases of pelvic inflammatory disease occur annually as a result of untreated chlamydia and gonorrhea, and four million women per year progress from pelvic inflammatory disease to infertility. Treating all women infected with chlamydia and gonorrhea would eliminate all pelvic inflammatory disease resulting from these infections, as well as the subsequent infertility; it would also avert the current cost of treating chlamydia- and gonorrhea-related pelvic inflammatory disease, which is an estimated $255 million annually (data not shown).
These cost estimates cover only treatment of the four major curable STIs in women aged 15–49 in LMICs. Costs associated with screening, diagnosis, vaccination and other preventive measures for these and other STIs are not included (except for those included in contraceptive, pregnancy-related and newborn care, which are costed separately). Moreover, the critical needs of some groups are not examined here, including populations at especially high risk for STIs, such as sex workers, people living in humanitarian crisis settings (see Box 6.1) and women outside of the 15–49 age range. Men’s needs for STI care are also excluded from this analysis, although there has been growing recognition in recent years of the need for comprehensive care for men and boys, as well as for women and girls.78
Women of reproductive age represent only part of the global need for STI care. Yet, the benefits of addressing STIs among these women are significant because prompt and effective treatment can eliminate pelvic inflammatory disease and reduce infertility. In addition, fully meeting women’s needs for STI treatment would greatly reduce ill-health resulting from STI infections among men, women and children, and would prevent stillbirths and fetal and newborn deaths caused by untreated syphilis.149
Cervical cancer
Cancer is a growing concern in LMICs. For several years now, throughout Asia and Latin America and in some countries in Africa, deaths from breast and cervical cancer have outnumbered deaths due to complications from pregnancy.150 Deaths from cervical cancer are almost entirely preventable. In 2018, about 570,000 women were diagnosed with cervical cancer worldwide; 311,000 died, the vast majority of whom lived in LMICs.151 Numbers of deaths were highest in South-Central and Eastern Asia, but the highest incidence rates were in Sub-Saharan Africa and parts of Oceania (Figure 6.2).
Cervical cancer is mainly caused by persistent infection with one or more of the high-risk genital subtypes of HPV.152 Most HPV infections resolve on their own, but some can lead to precancerous cervical lesions, which if not treated, can progress to cancer in 10–20 years. Among women living with HIV, the progression to cancer is often faster.153
Women diagnosed with cervical cancer need costly care that is often out of reach in LMICs. Fortunately, low-cost methods exist to prevent progression to cancer.154 WHO recommends screening women aged 30–49 for precancerous lesions at least once.152 Women living with HIV should be screened upon learning their HIV status and again every three years. Precancerous cervical lesions can often be treated through a low-cost, same-day procedure.154
Despite the availability of technologies for detecting and treating precancerous lesions, some of which are very low cost, access to these technologies is limited in many areas of the world, particularly where they are needed most. Primary prevention of HPV offers an opportunity to intervene earlier in women’s lives. Vaccination against the major cancer-causing types of HPV became possible more than a decade ago. WHO recommends giving highest priority for vaccination against HPV to girls aged 9–14;152 guidelines are also evolving in some locations to include adolescent boys.155 As of March 2017, 71 countries worldwide had national HPV immunization programs for girls; 11 countries also had programs for boys.143 However, programs are still notably absent in many LMICs, particularly in Africa and Asia.147
In a 2017 study focused on 50 LMICs, HPV vaccination and the screening and treatment of precancerous lesions were found to be very cost-effective interventions, at roughly $11.50 per woman reached (based on a three-dose vaccination regimen).156 These programs, when scaled up to meet need, could avert millions of deaths annually. Yet, for many countries, the ability to provide the necessary level of services is still several years away. A key challenge has been getting the vaccine at prices countries can afford, but as manufacturing costs decline over time, the vaccine should become more affordable everywhere.157 In the future, the HPV vaccine will be by far the most important intervention for reducing cervical cancer: WHO estimates that vaccination of more than 80% of girls aged 9–14, with no change in screening, could eliminate cervical cancer in most countries.158
HIV
According to the Joint United Nations Programme on HIV/AIDS, 38 million people in 2018 were living with HIV worldwide, including two million who were newly infected that year.140 Giant strides have been made over the last decade in HIV care and treatment; in particular, the expansion of access to antiretroviral therapy worldwide has changed the course of the HIV/AIDS epidemic. The therapy typically consists of a combination of antiretroviral medicines that suppress the virus, enabling people with HIV to live longer and reducing rates of transmission. Nevertheless, gaps remain in access to this lifesaving care, and the burden of disease is still disproportionately borne by women, particularly young women.
Women’s heightened vulnerability to infection. Due to a host of biological, sociocultural and economic reasons, young women and girls have much higher HIV infection rates than do young men and boys.159 Globally in 2018, there were an estimated 310,000 new infections among young women aged 15–24, compared with 200,000 among young men in the same age-group.160 More than four in five newly infected young women live in Sub-Saharan Africa.
In 2014, the global health community redoubled its prevention and treatment efforts for men and women by launching new targets. Referred to as 90-90-90, they call for ensuring that 90% of people living with HIV know their status, 90% of those individuals receive treatment and 90% of those on treatment are virally suppressed by 2020.161 Supporting these new targets, in 2015, WHO revised its HIV treatment guidelines to recommend immediate treatment with antiretroviral medicines upon diagnosis.162 With the support of global leaders and significant efforts at the international and country levels, at the end of 2018, the world had achieved 79–78–86.140
The 90-90-90 goals and the revised treatment guidelines do not specifically target women and girls, and it is unclear whether these advances will reduce women’s disproportionate share of HIV infections. However, another recent shift in HIV care and treatment may help to address this disparity. In 2015, alongside the revised treatment guidelines, WHO released guidance on offering oral preexposure prophylaxis, or PrEP, which is a combination of antiretroviral medicines shown to be effective and safe for daily use to prevent HIV infection.163 WHO recommended PrEP for "priority populations," such as sex workers, men who have sex with men and people who inject drugs. In settings with generalized HIV epidemics, the priority populations may also include young people, adolescents and women.164
As of mid-2018, 47 countries had approved the distribution of PrEP, and 39 countries had included it in their national HIV policies.165 However, actual availability and uptake of PrEP remains very low, and programs vary depending on characteristics of local epidemics. Countries in Sub-Saharan Africa, for example, are aiming to increase PrEP use among young women and girls, while programs in Southeast Asia are mainly targeting men who have sex with men.164
HIV’s impact on women’s health and lives. With increasing access to and use of antiretroviral treatment, people with HIV are living longer, shifting perceptions of HIV from an acute, life-threatening infection to a chronic health condition requiring management over time. This change toward managing HIV as a chronic health condition is particularly important for women because HIV affects many aspects of their sexual and reproductive health. Recognizing this fact, in 2017, WHO released guidelines on sexual and reproductive health care for women living with HIV.166
Achieving desired fertility is a particularly fraught issue for women living with HIV. They may experience reduced fertility,167 and they may require special counseling or medical intervention to achieve pregnancy safely. For women living with HIV who want to delay a birth or stop having children, health care providers must understand the complex drug interactions between hormonal contraceptives and antiretroviral regimens.168
A growing body of work also highlights the connections between the HIV epidemic and gender-based violence. The factors associated with women’s risk of experiencing violence perpetrated by an intimate partner predispose them to HIV infection.169 Many women who experience forced sex report being unable to negotiate condom use. Intimate partner violence, including emotional abuse, is also associated with faster disease progression among women living with HIV.170
HIV infection can also affect other reproductive health conditions. For example, as noted above, HIV increases women’s risk of HPV infection;153 also, women living with HIV may experience menopause earlier and have more symptoms.171–174 WHO emphasizes that women living with HIV have special needs during antenatal and postnatal care, and that they need access to safe abortion services, as well as services for preventing and managing other STIs.166
Intimate partner violence
Worldwide, nearly one-third of women experience intimate partner violence—defined as physical, sexual or emotional abuse from an intimate partner—in their lifetime.127 Often, it begins early in life: Twenty-nine percent of adolescent women aged 15–19 report having experienced violence from an intimate partner. Women who have experienced such violence are more likely than other women to have physical and mental health problems and to attempt suicide.127 Health consequences include depression, posttraumatic stress disorder, anxiety, self-harm, sleep disorders, chronic pain, gynecologic problems and increased risk of HIV and other STIs.175 Intimate partner violence affects every element of sexual and reproductive health reviewed in this report. More broadly, violence against women has profound impacts on households and society.176 Stemming from deep-seated gender inequality, it hinders social and economic progress at all levels.4
Interventions exist to prevent and respond to intimate partner violence, but broad implementation has been slow. Programs with proven effectiveness include microfinance initiatives for women that involve training aimed at transforming gender roles and relationships, community interventions to change social norms, and group education for men and boys.177–179 Protective orders and shelters have also been shown to be promising approaches.180
Addressing intimate partner violence and all forms of violence against women requires a coordinated multisectoral response.181 The main role of health care systems is to provide supportive care for women and their children facing the health effects of violence. Yet the health system also has a role in stopping and preventing violence, by documenting its occurrence and health consequences and by advocating coordinated action with other sectors.181 Responses to violence against women must also directly address persistent, harmful gender norms and attitudes.182
The costs of interventions to address violence against women are hard to measure, however, because existing approaches are often multisectoral, and most have been implemented on a small scale, without formal costing studies. Only a handful of studies from LMICs have determined the cost or economic value of interventions in terms of impacts, and because the costing approaches and program outcomes differ, the relative efficiency of the programs cannot be easily compared.183 However, more rigorous, coordinated analysis of the cost of interventions is underway in several locations across a number of LMICs.177,184
The United Nations Population Fund has called for an end to gender-based violence and recently released an analysis of the magnitude of resources needed to achieve that. They estimate that the cost of implementing a range of prevention and treatment programs to end gender-based violence in 132 countries by 2030 would be $42 billion.185 Such investments must cover the full range of service needs. In 2015, a joint United Nations program published the Essential Services Package for Women and Girls Subject to Violence, outlining guidelines for the core services to be provided by the health, social services, police and justice sectors.186
Infertility
Infertility is a central issue in the lives of many who experience it.187 Together with the relatively low political priority afforded this issue in LMICs, the high costs of diagnosis, treatment and assisted reproductive technologies have resulted in a huge divide between wealthy and poor countries in the availability of fertility care. Much more could be done, however, to raise awareness about and prevent infertility, to research low-cost solutions and to make access to new technologies more equitable across the globe.4
In addition to supporting people’s reproductive rights, which include the ability to choose whether and when to have children, there is a strong public health rationale for addressing infertility. Research has shown that infertility is associated with psychological distress, intimate partner violence and risky sexual behaviors, as well as social consequences such as stigma and exclusion, marital instability and economic hardship.188–191 While both men and women can experience infertility, in relationships, women are often blamed and bear the most severe consequences.192
The need for infertility services. Infertility, defined as the failure to achieve a pregnancy after 12 months or more of regular unprotected sexual intercourse,193 affected an estimated 5–15% of couples worldwide, as of 2006.194 Even higher prevalence rates are reported in parts of Sub-Saharan Africa.192,195 In 2012, WHO analyzed 277 health surveys and estimated that 49 million couples worldwide were suffering from infertility, half of whom were in Sub-Saharan Africa and Southern Asia.196
Factors that contribute to infertility include age and reproductive tract infections, as well as genetic, lifestyle and environmental factors.197 In LMICs, major causes include untreated gonorrhea and chlamydia, postabortion infections (which mainly result from unsafe abortions) and postpartum infections. HIV infection may also reduce fertility.198 Secondary infertility, the inability to become pregnant after having had a birth, has largely preventable and treatable causes, and it is more common worldwide than primary infertility, the inability to conceive a child at all.196
Prevention and treatment options. Prevention of infertility can begin by reducing risk factors for the condition. Interventions include comprehensive sexuality education; STI prevention, including condom use, and treatment; and counseling on fertility awareness to improve understanding of the optimal timing of sexual intercourse to achieve pregnancy.4 Health education programs can target factors known to be associated with infertility, such as tobacco and alcohol use, nutrition and occupational exposure to certain chemicals. Secondary infertility can be reduced through access to safe delivery and safe abortion care, and through prevention, detection and treatment of STIs. Primary health care providers can counsel clients on infertility, especially to dispel some of the myths and misperceptions about infertility197 and to refer affected couples to more specialized care.
Treatment options for infertility, which depend on resource availability, include drugs to induce ovulation, intrauterine insemination, surgery to address abnormalities (such as blocked fallopian tubes) and assisted reproductive technologies.199 Specific populations, including LGBTQ people and people living with medical conditions such as HIV or cancer, may especially need these types of care.
The availability and quality of interventions to address infertility are extremely limited in LMICs. Even basic interventions—counseling, medical examinations and information on infertility and treatment options—are often absent.197 Advanced treatment of infertility using assisted reproductive technologies requires highly skilled labor and expensive equipment, which are often not available in LMICs, and such treatment is usually not included as part of essential health care.
Lower cost fertility drugs and a simpler and less expensive laboratory method for in vitro fertilization are starting to become available, which will greatly increase access to assisted reproductive technologies in LMICs.200 International partnerships, including South-South cooperation, can help ensure that clinicians and laboratory scientists in LMICs establish and maintain high-quality services.195 Launching and expanding these efforts worldwide may require a global initiative, with high-level support and international funding, to transfer knowledge and affordable technologies to LMICs. For now, the key starting points for helping millions of couples affected by infertility are to raise awareness about the issue, reduce the stigma surrounding it, focus on prevention and counsel couples about their options.201
Box 6.1
Sexual and reproductive health services in humanitarian settings
In 2018, there were roughly 71 million forcibly displaced people worldwide, a record high; about half of these individuals were women and girls.202 Providing humanitarian assistance where needed—in areas affected by conflict, natural disasters or other emergencies—is challenging, and lifesaving care must be prioritized. There is also growing recognition of the need to address the sexual and reproductive health needs of individuals in these settings. Adolescent women, in particular, face increased risk of sexual assault and other forms of gender-based violence, trafficking and child marriage.203 The erosion of health care services (including contraceptive care) during crises, combined with elevated levels of sexual violence, can lead to increases in unintended pregnancies, unsafe abortions, and transmission of HIV and other STIs.204,205
The Inter-Agency Field Manual on Reproductive Health in Humanitarian Settings, revised in 2018, provides comprehensive guidance on sexual and reproductive health service provision.205 The manual contains a Minimum Initial Service Package, which highlights the most vital services for settings with minimal resources and gives guidance to humanitarian workers and first responders on transitioning from an initial response to providing comprehensive care. The guidance calls for services to respect clients’ rights to nondiscrimination and quality care.
The field manual also addresses a number of formidable service weaknesses. Humanitarian aid programs rarely provide a full range of contraceptive options, and the greatest gaps in availability are for long-acting reversible contraceptives and sterilization.206 Condoms tend to be more widely available, partly due to the success of past initiatives focused on HIV prevention in these settings.207 The greatest progress has occurred in maternal and newborn health care, but treatment gaps remain for emergency obstetric care, newborn infection care and assisted vaginal delivery.206,207 Safe abortion services and postabortion care are largely unavailable in humanitarian settings. Most humanitarian organizations and health facilities do not provide abortion for a variety of reasons, including legal prohibitions, incorrect assumptions about abortion legality, misperceptions about the need for it, concerns that abortion procedures are too complicated to be provided under resource-limited conditions, and insufficient funding.204,206
Looking forward, improving training in sexual and reproductive health for health workers in these settings is vital.206 The demand for comprehensive clinical management of rape is particularly high.207 Services are needed not only for women and girls but for men and boys, who—because of stigma, shame and inadequate health worker training—often receive insufficient and poor-quality care after experiencing a sexual assault.208 Systems for ensuring a consistent supply of contraceptive commodities, drugs and supplies are also critical, as providers often cite shortages as key barriers to service provision.206,209 Special considerations must be made at the onset of a response to ensure the continuous availability of needed supplies.207
Questions about who is responsible for providing specific services and who should pay are often unresolved in humanitarian settings. The deterioration of health care infrastructure and weakening or loss of the systems for managing care, particularly state-run systems, are common in countries with many people living in fragile settings.210 As camps for refugees and displaced persons reach capacity, service quality within camps may erode over time, and health worker shortages and poor coordination among state, private and humanitarian service organizations may exacerbate these issues.206,207,211 Better planning and coordination are needed, yet the cost of providing quality, comprehensive care in these settings is not well understood.212 Much existing research has focused on determining the most cost-effective interventions and efficient modes of service delivery, rather than considering the total costs and requirements for an integrated approach across the protection, health and nutrition sectors. As countries progress toward universal health coverage, more information is needed on the health system costs and the roles and responsibilities of various entities in responding to service needs in humanitarian settings.
7. Conclusions
This report shows why investing in sexual and reproductive health care is essential for people’s well-being and constitutes good public policy. As cornerstones of a healthy and satisfying life, sexual and reproductive health and rights are intertwined with human rights.4 Moreover, many of the services examined here are essential for achieving universal health coverage in that they address a significant health burden, provide good value for money and have proven feasible to implement.213 As with other types of health care, the greatest unmet needs for sexual and reproductive health care are concentrated in the poorest countries and among the most marginalized people.
As of 2019, 705 million women in LMICs rely on modern contraceptives, and 218 million more want to avoid a pregnancy but are not using a modern method.45 An estimated 111 million experience an unintended pregnancy each year. Tens of millions of women receive inadequate care during pregnancy and delivery, as well as after a birth, abortion, miscarriage or stillbirth, resulting in needless death and disability. An estimated 133 million women of reproductive age do not receive the treatment they need for the four major curable STIs. Contraceptive, pregnancy-related and STI care must expand and improve to fully meet women’s service needs and avert the negative health consequences that result from difficulties obtaining services and low-quality care.
The data in this report illustrate the magnitude of the impact that would result from fully investing in meeting these needs immediately. Conversely, the data reveal the cost of inaction, in terms of lives lost and diminished human potential.
Gains from meeting sexual and reproductive health needs
Fulfilling all unmet needs for modern contraception and providing essential health services for all pregnant women and newborns would result in substantial improvements in health in LMICs:
- Unintended pregnancies would drop by 68%, from 111 million to 35 million
- Unplanned births would drop by 71%, from 30 million to nine million
- Unsafe abortions would drop by 72%, from 35 million to 10 million
- Maternal deaths would drop by 62%, from 299,000 to 113,000
Providing the recommended maternal and newborn care would also vastly improve newborn health. Newborn deaths would drop by 69%, from 2.5 million to 0.8 million, and new HIV infections among babies six weeks and younger would drop by 88%, from 110,000 to 14,000.
In addition, treating all women infected with chlamydia and gonorrhea would eliminate 30 million cases of pelvic inflammatory disease and three million cases of infertility caused by these STIs.
Evidence from other studies also shows that beyond saving lives and improving people’s health and well-being, sexual and reproductive health care can boost productivity and income—for individuals, families and countries (see Box 4.1). The benefits are multigenerational in that these services also improve children’s health and well-being. For adolescents, receiving the sexual and reproductive health services they need helps them have fewer unintended pregnancies, unplanned births and unsafe abortions, and results in healthier outcomes for adolescent mothers and their children—all of which can affect the long-term trajectory of their lives. Investing in sexual and reproductive health services pays dividends over many years and makes it easier for countries to achieve other development goals.
The investments needed to achieve these gains
Meeting all needs in LMICs for modern contraception, pregnancy-related and newborn care, and STI services would cost $68.9 billion annually, $31.2 billion more than the cost of current services (Table 7.1).45 The total investment needed, which includes both direct costs and programs and systems costs, translates to approximately $10.60 per capita per year, or about $4.80 per capita more than current costs. This investment would expand the provision of services to all who need them and ensure that all users receive services that meet World Health Organization (WHO) standards for quality of care.
The total reflects the cost savings that would result from investing simultaneously in contraceptive services and pregnancy-related and newborn care, rather than investing in pregnancy-related and newborn care alone. Investing $5.5 billion annually to provide modern contraceptives to all women who need them would reduce the cost of pregnancy-related and newborn care by $16.3 billion (as described in Chapter 4). In other words, every dollar spent on contraceptive services beyond the current level would reduce the cost of pregnancy-related and newborn care by three dollars.
In this combined package of care, the major components of maternal and newborn care together amount to 76% (Figure 7.1). Contraception accounts for about one-fifth of the total. Treatment of the four major curable STIs not given during pregnancy and abortion services account for only 3% and 2%, respectively.
To put the $10.60 per capita in context, a study examining total per capita health expenditure found that spending ranged from $40 per capita in low-income countries to $491 per capita in upper-middle–income countries—amounts that were projected to rise substantially as countries place greater priority on improving health care.214 In our analysis, the additional investment required to move from current levels of care to immediate, full coverage of sexual and reproductive health care is about $4.80 per capita per year on average across LMICs.45 This amount represents only a small fraction of the additional health care spending that will be required to meet the health-related Sustainable Development Goals.62
Programs and systems costs account for the majority of total costs in this analysis (64% of the required investment in LMICs as a whole; data not shown).45 Expanding service coverage and improving quality of care requires functional health systems. The programs and systems costs reflect the need for additional resources for expanding infrastructure and increasing numbers of trained staff, as well as improving vital logistics and health information systems. Strengthening the foundation of sexual and reproductive health care in these ways would also benefit the health system more broadly.
Although this analysis focuses on financial investments, money alone will not ensure all women’s sexual and reproductive health care needs are met. Other studies shed light on wide-ranging obstacles to satisfying all needs for such care.4,42 For example, in some countries, policies and regulations restrict access to contraceptives, safe abortion services and other sexual and reproductive health services. Shortages of skilled health workers are also common in LMICs, and the current workforce may not be deployed in the areas where it is most needed. Moreover, biases among health providers can prevent them from extending quality services to all clients;53 for instance, unmarried young people, people living in poverty, people with disabilities, members of minority ethnic groups and LGBTQ people often experience discriminatory treatment. More broadly, social and cultural attitudes that reinforce gender inequality, limit women’s empowerment and mobility, and stigmatize HIV, abortion and other sexual and reproductive health issues, can reduce people’s demand for and access to care.4
Therefore, linking efforts to improve sexual and reproductive health services with policies and programs in other sectors, such as education, social welfare and the justice system, could bring about greater gains in health to women, their families and societies. We have not estimated the costs of these complementary investments in our analysis, but we intend that financing decisions related to sexual and reproductive health will occur as part of a broader strategy to improve people’s health and well-being.
Meeting other sexual and reproductive health needs
Increased investments in other areas of sexual and reproductive health are not included in our estimates of costs and benefits but would also improve the health and well-being of women and their families. Proven interventions exist to prevent and treat cervical cancer, HIV and infertility, and to respond to intimate partner violence, but the degree to which they have been introduced and scaled up varies greatly across countries. The Guttmacher-Lancet Commission on Sexual and Reproductive Health and Rights proposes offering all people an essential package of interventions that includes all of the components of sexual and reproductive health care reviewed in this report, as part of universal health coverage.4
The magnitude of needs is too large to ignore. Cervical cancer, for example, kills 311,000 women every year worldwide, the vast majority of whom are in LMICs151—despite the fact that it can be prevented with proven, low-cost interventions. Ramped-up investments in HPV vaccination, and screening and treatment of cervical precancer are long overdue. Also, HIV remains a major cause of disability and death worldwide, and young women still account for a disproportionate share of new HIV infections among young people.160 Although progress has been made to curb the global pandemic, the job is not done.
We have insufficient information to calculate the costs of services to respond to intimate partner violence and infertility, even though these concerns are central to the well-being of those affected. Intimate partner violence is widespread, affecting nearly one in three women worldwide during their lifetime,127 and access to services to address infertility, which affects 5–15% of couples worldwide,194 is vastly inequitable between the wealthy and the poor.
Paying for improved services
The dollar amounts shown in Table 7.1 represent the costs to the whole health system of providing selected sexual and reproductive health services to all women in LMICs who need them, regardless of who pays. Where would the funds come from to expand and improve services?
Globally, discussions about universal health coverage continue to grapple with questions about the affordability of care and who should pay for it. In wealthier countries, government revenues and pooled contributions (insurance) cover most health care expenses and thus help minimize financial risks for individuals.214 However, out-of-pocket spending tends to be proportionally highest in the poorest countries: In 2017, it accounted for an estimated 40% of current health expenditure in low-income countries, compared with 22% in high-income countries.215 As a result, people who can least afford it pay for much of their care out of pocket. Adolescents are particularly impacted by out-of-pocket contributions to health care because they often are not financially independent, and confidentiality and other concerns may prevent them from using their families’ resources.216
Development assistance for health makes up about 25% of health spending in low-income countries; in some, it accounts for more than 50%.217 Middle-income countries have already increased their domestic government and private-sector financing of health, and similar increases will be critical over the long term in low-income countries.214 For the near future, however, increased domestic spending alone is not likely to close the gaps in services.
In fact, no single source of funding will fill the existing gaps in care. Modes of financing may vary, but a key objective of universal health coverage is to ensure that essential health services are accessible to everyone needing care and that their use does not cause financial hardship.1,218 Attaining universal access will entail increasing the share of costs covered by pooled contributions, thereby reducing reliance on out-of-pocket payments that deter those most in need from receiving care.62 In countries with high health burdens and limited domestic budgets, external donor funding and effective partnerships between donors and recipient countries will continue to be necessary for expanding and improving services.
Getting to full care
The speed at which countries can move toward universal coverage of high-quality sexual and reproductive health care will vary greatly, depending on their starting point and their capacity for making needed improvements. For the package of care presented here, the additional investment over current levels is largest in low-income countries because these countries have the highest unmet needs and their health systems require the most strengthening to provide the recommended care.45
The need for additional funds is highest in Western and Eastern Africa and Southern Asia, followed by other parts of Africa and Asia (Figure 7.2). Of the $31.2 billion increase required for all LMICs to provide the full package of recommended care, $24.1 billion (or 77%) is needed in Sub-Saharan Africa and Southern Asia. At the other end of the spectrum, LMICs in South America and Eastern Europe require smaller increases because they have lower unmet needs for services, and the savings that accrue from reducing unintended pregnancies offset the necessary improvements in the service package.
The required increases highlight the size of current gaps and the resources required to close them. No country will attain full coverage immediately. Rather, countries will likely need to work in a stepwise fashion to assess high-priority needs and allocate resources in ways that ensure access to needed care for those least able to pay.4 In this way, they can make substantial progress toward realizing sexual and reproductive health and rights as part of their efforts to achieve universal health coverage and related SDG targets by 2030.62
Because these changes are not quick fixes, sustained efforts are essential. The necessary commitments include long-term, predictable funding; support for evidence-based programs and services; and an emphasis on equity—that is, devoting sufficient resources to increase access to high-quality care for those who have the greatest needs.62 A human rights approach to health is essential for a shift in focus toward poor and marginalized groups, and it is also necessary for achieving universal health coverage as envisioned in the SDGs. The health-related SDGs and other global initiatives, such as the Global Strategy on Women’s, Children’s and Adolescents’ Health, have consistently emphasized universality and equity in health care.
Some of the changes called for in this report are less measurable but no less important—namely, fostering a health care culture that values individual choice and well-being and ends all forms of discrimination against individuals who need sexual and reproductive health services. The ability to decide whether and when to have children, to have a healthy pregnancy and newborn, and to have a safe, healthy and pleasurable sexual life should not be limited to privileged groups of individuals. These are fundamental rights for all people. Investments in sexual and reproductive health care result in benefits that ripple across communities and countries and multiply over generations—and conversely, the failure to invest robs current and future generations of the potential to thrive.
FOOTNOTES
*American Samoa, Dominica, Marshall Islands, Nauru and Tuvalu. Following UN Population Division classifications, Kosovo is collapsed with Serbia for all calculations.
†Use of the 30-day cut-off produces minimum estimates of the number of women wanting to avoid pregnancy and the need for contraception. Other definitions of "current" sexual activity (e.g., sex in the last three months, last year or ever) result in larger proportions of unmarried women classified as sexually active.
‡This report uses the revised 2017 WHO definition of abortion safety.25 Safe abortions are those that use a WHO-recommended method appropriate to the pregnancy duration and are done by a trained provider. Less safe abortions meet only one of these criteria, and least safe abortions meet neither criterion. We use "unsafe" to refer to both less safe and least safe abortions.
§Defined as fetal deaths before 28 weeks’ gestation.30
**Defined as babies born with no signs of life at or after 28 weeks’ gestation.30
††All cost estimates in this report are one-year estimates in 2019 U.S. dollars.
‡‡Oral contraceptive pill, injectable, patch, ring and emergency contraception.
§§Because this report focuses on maternal and newborn health during pregnancy and for approximately six weeks after birth, it excludes the cost of antiretroviral therapy for women who were receiving it prior to pregnancy, even if they continue to receive it while pregnant and postpartum. This report also excludes antiretroviral therapy costs for women beyond six weeks postpartum and for infants older than six weeks.
*†Country-level data were used for Bangladesh,26 Ethiopia,27 India28 and Nepal.29
*‡Use of the 30-day cut-off produces minimum estimates of the number of women wanting to avoid pregnancy and the need for contraception. Other definitions of "current" sexual activity (e.g., sex in the last three months, last year or ever) result in larger proportions of unmarried women classified as sexually active.
REFERENCES
1. United Nations (UN), Transforming Our World: The 2030 Agenda for Sustainable Development, 2015, No. A/RES/70/1, https://sustainabledevelopment.un.org/post2015/transformingourworld/pub….
2. Family Planning 2020 (FP2020), FP2020: Women at the Center 2018–2019, 2019, http://progress.familyplanning2020.org/.
3. Every Woman Every Child, Global Strategy for Women’s, Children’s and Adolescents’ Health 2016–2030, New York: UN, 2015, http://www.who.int/life-course/publications/global-strategy-2016-2030/e….
4. Starrs AM et al., Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher–Lancet Commission, Lancet, 2018, 391(10140):2642–2692, doi:10.1016/S0140-6736(18)30293-9.
5. World Bank, World Bank country and lending groups (2020 fiscal year), 2019, https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-….
6. Population Division, UN Department of Economic and Social Affairs, World Population Prospects 2019, Online Edition. Rev. 1, 2019, https://population.un.org/wpp/Download/Standard/.
7. Singh S et al., Adding It Up: The Benefits of Investing in Sexual and Reproductive Health Care, New York: The Alan Guttmacher Institute and United Nations Population Fund (UNFPA), 2003, https://www.guttmacher.org/report/adding-it-benefits-investing-sexual-a….
8. Singh S et al., Adding It Up: The Costs and Benefits of Investing in Family Planning and Maternal and Newborn Health, New York: Guttmacher Institute and UNFPA, 2009, https://www.guttmacher.org/report/adding-it-costs-and-benefits-investin….
9. Singh S and Darroch JE, Adding It Up: Costs and Benefits of Contraceptive Services—Estimates for 2012, New York: Guttmacher Institute, 2012, https://www.guttmacher.org/report/adding-it-costs-and-benefits-contrace….
10. Singh S, Darroch JE and Ashford LS, Adding It Up: The Need for and Cost of Maternal and Newborn Care–Estimates for 2012, New York: Guttmacher Institute, 2013, https://www.guttmacher.org/report/adding-it-need-and-cost-maternal-and-….
11. Singh S, Darroch JE and Ashford LS, Adding It Up: The Costs and Benefits of Investing in Sexual and Reproductive Health 2014, New York: Guttmacher Institute, 2014, https://www.guttmacher.org/report/adding-it-costs-and-benefits-investin….
12. Guttmacher Institute, Adding It Up: investing in contraception and maternal and newborn health, 2017, Fact Sheet, New York: Guttmacher Institute, 2017, https://www.guttmacher.org/fact-sheet/adding-it-up-contraception-mnh-20….
13. Institute for International Programs, Bloomberg School of Public Health, Johns Hopkins University, The Lives Saved Tool, Spectrum Version 5.73, no date, https://www.livessavedtool.org/listspectrum.
14. UN Inter-Agency Working Group on Costing, OneHealth Tool, no date, https://www.avenirhealth.org/software-onehealth.php.
15. Serje J et al., Global health worker salary estimates: an econometric analysis of global earnings data, Cost Effectiveness and Resource Allocation, 2018, 16(10), doi:10.1186/s12962-018-0093-z.
16. UNFPA Procurement Services, RHInterchange, 2020, https://www.unfpaprocurement.org/rhi-home.
17. UNFPA Procurement Services, UNFPA Product Catalog, 2019, https://www.unfpaprocurement.org/products.
18. United Nations Children’s Fund (UNICEF), UNICEF Supply Catalogue, 2018 https://supply.unicef.org/.
19. Management Sciences for Health, International Medical Products Price Guide, 2016, http://mshpriceguide.org/en/home/.
20. IDA Foundation, Product Indicator 2019, 2019, https://www.idafoundation.org/media/wysiwyg/products/IDA_Product_Indica….
21. UNFPA Technical Division, Revised Cost Estimates for the Implementation of the Programme of Action for the International Conference on Population and Development: A Methodological Report, New York: UNFPA, 2009.
22. Population Division, UN Department of Economic and Social Affairs, Estimates and projections of family planning indicators 2020, 2020, https://www.un.org/en/development/desa/population/theme/family-planning….
23. Bearak JM et al., Pregnancies, abortions, and pregnancy intentions: a protocol for modeling and reporting global, regional and country estimates, Reproductive Health, 2019, Vol. 16, No. 36, doi:10.1186/s12978-019-0682-0.
24. Bearak J et al., Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990–2019, Lancet Global Health, 2020, 8(9), http://www.thelancet.com/journals/langlo/article/PIIS2214-109X(20)30315-6/fulltext.
25. Ganatra B et al., Global, regional, and subregional classification of abortions by safety, 2010–14: estimates from a Bayesian hierarchical model, Lancet, 2017, 390(10110):2372–2381, doi:10.1016/S0140-6736(17)31794-4.
26. Singh S et al., The incidence of menstrual regulation procedures and abortion in Bangladesh, 2014, International Perspectives on Sexual and Reproductive Health, 2017, 43(1):1–11, doi:10.1363/43e2417.
27. Moore AM et al., The estimated incidence of induced abortion in Ethiopia, 2014: changes in the provision of services since 2008, International Perspectives on Sexual and Reproductive Health, 2016, 42(3):111–120, doi:10.1363/42e1816.
28. Singh S et al., The incidence of abortion and unintended pregnancy in India, 2015, Lancet Global Health, 2018, 6(1):e111–e120, doi:10.1016/S2214-109X(17)30453-9.
29. Puri M et al., Abortion incidence and unintended pregnancy in Nepal, International Perspectives on Sexual and Reproductive Health, 2016, 42(4):197–209, doi:10.1363/42e2116.
30. Blencowe H et al., National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systemic analysis, Lancet Global Health, 2016, 4(2):e98–e108, doi:10.1016/S2214-109X(15)00275-2.
31. Leridon H, Human Fertility: The Basic Components, Chicago: University of Chicago Press, 1977, Table 4.20.
32. WHO, special tabulations of data from Maternal Mortality, Levels and Trends 2000 to 2017, 2019, http://mmr2017.srhr.org/.
33. Institute for Health Metrics and Evaluation (IHME), Global Burden of Disease Study 2017 Results, 2018, http://ghdx.healthdata.org/gbd-results-tool.
34. World Health Organization (WHO) Department of Evidence, Information and Research and Maternal Child Epidemiology Estimation, MCEE-WHO methods and data sources for child causes of death 2000–2017, Global Health Estimates Technical Paper, 2018.
35. Bradley S et al., Global contraceptive failure rates: Who is most at risk?, Studies in Family Planning, 2019, 50(1):3–24, doi:10.1111/sifp.12085.
36. Trussell J, Contraceptive failure in the United States, Contraception, 2011, 83(5):397–404, doi:10.1016/j.contraception.2011.01.021.
37. Arévalo M, Jennings V and Sinai I, Efficacy of a new method of family planning: the Standard Days Method, Contraception, 2002, 65(5):333–338, doi:10.1016/S0010-7824(02)00288-3.
38. Van der Wijden C and Manion C, Lactational amenorrhoea method for family planning, Cochrane Database of Systematic Reviews, 2015, (10), doi:10.1002/14651858.CD001329.pub2.
39. Darroch JE, Adding It Up: Investing in Contraception and Maternal and Newborn Health, 2017—Estimation Methodology, New York: Guttmacher Institute, 2018, https://www.guttmacher.org/report/adding-it-up-investing-in-contracepti….
40. Rowley J et al., Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016, Bulletin of the World Health Organization, 2019, 97:584–562P, doi:10.2471/BLT.18.228486.
41. WHO, Sexually transmitted infections (STIs), Fact Sheet, 2019, https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis).
42. Stenberg K et al., Advancing social and economic development by investing in women’s and children’s health: a new Global Investment Framework, Lancet, 2014, 383(9925):1333–1354, doi:10.1016/S0140-6736(13)62231-X.
43. Canning D and Schultz TP, The economic consequences of reproductive health and family planning, Lancet, 2012, 380(9837):165–171, doi:10.1016/S0140-6736(12)60827-7.
44. Ashraf QH, Weil DN and Wilde J, The effect of fertility reduction on economic growth, Population and Development Review, 2013, 39(1):97–130, doi:10.1111/j.1728-4457.2013.00575.x.
45. Adding It Up 2019 analysis.
46. Ueffing P, Dasgupta ANZ and Kantorová V, Sexual activity by marital status and age: a comparative perspective, Journal of Biosocial Science, 2019, doi:10.1017/S002193201900083X.
47. Bradley S et al., Revising unmet need for family planning, DHS Analytical Studies, Calverton, MD, USA: ICF International, 2012, No. 25, https://dhsprogram.com/pubs/pdf/AS25/AS25%5B12June2012%5D.pdf.
48. UN Department of Economic and Social Affairs, Statistics Division, SDG Indicators, no date, https://unstats.un.org/sdgs/indicators/indicators-list/.
49. Sully EA, Biddlecom A and Darroch JE, Not all inequalities are equal: differences in coverage across the continuum of reproductive health services, BMJ Global Health, 2019, 4, doi:10.1136/bmjgh-2019-001695.
50. Victora CG et al., The contribution of poor and rural populations to national trends in reproductive, maternal, newborn, and child health coverage: analyses of cross-sectional surveys from 64 countries, Lancet Global Health, 2017, 5(4):e402–e407, doi:10.1016/S2214-109X(17)30077-3.
51. Cleland J, Harbison S and Shah IH, Unmet need for contraception: issues and challenges, Studies in Family Planning, 2014, 45(2):105–122, doi:10.1111/j.1728-4465.2014.00380.x.
52. Sedgh G, Ashford L and Hussain R, Unmet Need for Contraception in Developing Countries: Examining Women’s Reasons for Not Using a Method, New York: Guttmacher Institute, 2016, https://www.guttmacher.org/report/unmet-need-for-contraception-in-devel….
53. Solo J and Festin M, Provider bias in family planning services: a review of its meaning and manifestations, Global Health: Science and Practice, 2019, doi:10.9745/GHSP-D-19-00130.
54. Ali M, Cleland J and Shah I, Causes and Consequences of Contraceptive Discontinuation: Evidence from 60 Demographic and Health Surveys, Geneva: WHO, 2012, https://apps.who.int/iris/bitstream/handle/10665/75429/9789241504058_en….
55. Jain AK et al., Reducing unmet need by supporting women with met need, International Perspectives on Sexual and Reproductive Health, 2013, 39(03):133–141, doi:10.1363/3913313.
56. Blithe DL, Pipeline for contraceptive development, Fertility and Sterility, 2016, 106(6):1295–1302, doi:10.1016/j.fertnstert.2016.07.1115.
57. Belaid L et al., Effectiveness of demand generation interventions on use of modern contraceptives in low- and middle-income countries, Tropical Medicine & International Health, 2016, 21(10):1240–1254, doi:10.1111/tmi.12758.
58. Mwaikambo L et al., What works in family planning interventions: a systematic review of the evidence, Studies in Family Planning, 2011, 42(2):67–82, doi:10.1111/j.1728-4465.2011.00267.x.
59. Rodriguez MI et al., Ensuring Human Rights in the Provision of Contraceptive Information and Services: Guidance and Recommendations, Geneva: WHO, 2014.
60. FP2020, Family Planning 2020: Rights and Empowerment Principles for Family Planning, no date, https://www.familyplanning2020.org/sites/default/files/FP2020_Statement….
61. Biddlecom A et al., Future Scenarios of Adolescent Contraceptive Use, Cost and Impact in Developing Regions, New York: Guttmacher Institute, 2018, https://www.guttmacher.org/report/adolescent-contraceptive-use-in-devel….
62. Stenberg K et al., Financing transformative health systems towards achievement of the health Sustainable Development Goals: a model for projected resource needs in 67 low-income and middle-income countries, Lancet Global Health, 2017, 5(9):e875–e887, doi:10.1016/S2214-109X(17)30263-2.
63. WHO et al., Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division, Geneva: WHO, 2019.
64. United Nations Inter-Agency Group for Child Mortality Estimation, Levels & Trends in Child Mortality: Report 2019, Estimates Developed by the United Nations Inter-Agency Group for Child Mortality Estimation, New York: UNICEF, 2019, https://childmortality.org/wp-content/uploads/2019/10/UN-IGME-Child-Mor….
65. Kruk ME et al., Mortality due to low-quality health systems in the universal health coverage era: a systematic analysis of amenable deaths in 137 countries, Lancet, 2018, 392(10160):2203–2212, doi:10.1016/S0140-6736(18)31668-4.
66. Kruk ME et al., Quality of basic maternal care functions in health facilities of five African countries: an analysis of national health system surveys, Lancet Global Health, 2016, 4(11):e845–e855, doi:10.1016/S2214-109X(16)30180-2.
67. Campbell OMR et al., The scale, scope, coverage, and capability of childbirth care, Lancet, 2016, 388(10056):2193–2208, doi:10.1016/S0140-6736(16)31528-8.
68. Starrs AM, Survival convergence: bringing maternal and newborn health together for 2015 and beyond, Lancet, 2014, 384(9939):211–213, doi:10.1016/S0140-6736(14)60838-2.
69. WHO, WHO Recommendations on Maternal Health: Guidelines Approved by the Guidelines Review Committee, 2017, https://apps.who.int/iris/bitstream/handle/10665/259268/WHO-MCA-17.10-e….
70. WHO, WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience, 2016, https://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-e….
71. WHO, UNFPA and UNICEF, Pregnancy, Childbirth, Postpartum and Newborn Care: A Guide for Essential Practice, Geneva: WHO, 2015, http://www.who.int/maternal_child_adolescent/documents/imca-essential-p….
72. Masi S de et al., Integrated person-centered health care for all women during pregnancy: implementing World Health Organization recommendations on antenatal care for a positive pregnancy experience, Global Health: Science and Practice, 2017, 5(2):197–201, doi:10.9745/GHSP-D-17-00141.
73. WHO et al., Managing Complications in Pregnancy and Childbirth: A Guide for Midwives and Doctors, second ed., 2017, https://apps.who.int/iris/bitstream/handle/10665/255760/9789241565493-e….
74. WHO, Standards for Maternal and Neonatal Care, 2007, https://apps.who.int/iris/bitstream/handle/10665/69735/a91272.pdf;seque….
75. Benova L et al., Not just a number: examining coverage and content of antenatal care in low-income and middle-income countries, BMJ Global Health, 2018, 3(2):e000779, doi:10.1136/bmjgh-2018-000779.
76. Joseph Davey D et al., Prevalence of curable sexually transmitted infections in pregnant women in low- and middle-income countries from 2010 to 2015, Sexually Transmitted Diseases, 2016, 43(7):450–458, doi:10.1097/OLQ.0000000000000460.
77. Medline A, Joseph Davey D and Klausner JD, Lost opportunity to save newborn lives: variable national antenatal screening policies for Neisseria gonorrhoeae and Chlamydia trachomatis, International Journal of STD & AIDS, 2016, 28(7):660–666, doi:10.1177/0956462416660483.
78. WHO, Global Health Sector Strategy on Sexually Transmitted Infections 2016–2021: Towards Ending STIs, 2016, https://apps.who.int/iris/bitstream/handle/10665/246296/WHO-RHR-16.09-e….
79. WHO, Global Guidance on Criteria and Processes for Validation: Elimination of Mother-to-Child Transmission of HIV and Syphilis, second ed., 2017, https://apps.who.int/iris/bitstream/handle/10665/259517/9789241513272-e….
80. WHO, WHO Guideline on Syphilis Screening and Treatment for Pregnant Women, 2017, http://www.who.int/reproductivehealth/publications/rtis/syphilis-ANC-sc….
81. Gülmezoglu A et al., Interventions to reduce maternal and newborn morbidity and mortality, in: Reproductive, Maternal, Newborn, and Child Health Disease Control Priorities, Third Edition (Volume 2), Washington, DC: World Bank, 2016, pp. 115–136, https://elibrary.worldbank.org/doi/full/10.1596/978-1-4648-0348-2_ch7.
82. Betran A et al., WHO statement on caesarean section rates, BJOG, 2016, 123(5):667–670, doi:10.1111/1471-0528.13526.
83. Boerma T et al., Global epidemiology of use of and disparities in caesarean sections, Lancet, 2018, 392(10155):1341–1348, doi:https://doi.org/10.1016/S0140-6736(18)31928-7.
84. Kozuki N and Walker N, Exploring the association between short/long preceding birth intervals and child mortality: using reference birth interval children of the same mother as comparison, BMC Public Health, 2013, 13(Suppl. 3):S6, doi:10.1186/1471-2458-13-S3-S6.
85. Conde-Agudelo A et al., Effects of birth spacing on maternal, perinatal, infant, and child health: a systemic review of causal mechanisms, Studies in Family Planning, 2012, 43(2):93–114, doi:10.1111/j.1728-4465.2012.00308.x.
86. High Impact Practices in Family Planning, Immediate Postpartum Family Planning: A Key Component of Childbirth Care, Washington, DC: U.S. Agency for International Development (USAID), 2017, https://www.fphighimpactpractices.org/briefs/immediate-postpartum-famil….
87. Lawn JE et al., Every newborn: progress, priorities, and potential beyond survival, Lancet, 2014, 384(9938):189–205, doi:10.1016/S0140-6736(14)60496-7.
88. UNAIDS, Start Free Stay Free AIDS Free, 2019, https://www.unaids.org/en/resources/documents/2019/20190722_UNAIDS_SFSF….
89. WHO, Safe Abortion: Technical and Policy Guidance for Health Systems, Second Edition, 2012, http://www.who.int/reproductivehealth/publications/unsafe_abortion/9789….
90. WHO, Medical Management of Abortion, 2018.
91. Souza JP et al., Moving beyond essential interventions for reduction of maternal mortality (the WHO Multicountry Survey on Maternal and Newborn Health): a cross-sectional study, Lancet, 2013, 381(9879):1747–1755, doi:10.1016/S0140-6736(13)60686-8.
92. Montagu D et al., Where women go to deliver: understanding the changing landscape of childbirth in Africa and Asia, Health Policy and Planning, 2017, 32(8):1146–1152, doi:10.1093/heapol/czx060.
93. Owolabi OO, Biddlecom A and Whitehead HS, Health systems’ capacity to provide post-abortion care: a multicountry analysis using signal functions, Lancet Global Health, 2019, 7(1):e110–e118, doi:10.1016/S2214-109X(18)30404-2.
94. Wang W et al., Effective coverage of facility delivery in Bangladesh, Haiti, Malawi, Nepal, Senegal, and Tanzania, PLOS ONE, 2019, 14(6):e0217853, doi:10.1371/journal.pone.0217853.
95. Bohren MA et al., The mistreatment of women during childbirth in health facilities globally: a mixed-methods systematic review, PLOS Medicine, 2015, 12(6):e1001847, doi:10.1371/journal.pmed.1001847.
96. Jewkes R and Penn-Kekana L, Mistreatment of women in childbirth: time for action on this important dimension of violence against women, PLOS Medicine, 2015, 12(6):e1001849, doi:10.1371/journal.pmed.1001849.
97. Bohren MA et al., Facilitators and barriers to facility-based delivery in low- and middle-income countries: a qualitative evidence synthesis, Reproductive Health, 2014, 11(1):71, doi:10.1186/1742-4755-11-71.
98. Bohren MA et al., How women are treated during facility-based childbirth in four countries: a cross-sectional study with labour observations and community-based surveys, Lancet, 2019, 394(10210):1750–1763, doi:10.1016/S0140-6736(19)31992-0.
99. Singh S et al., Abortion Worldwide 2017: Uneven Progress and Unequal Access, New York: Guttmacher Institute, 2018, https://www.guttmacher.org/report/abortion-worldwide-2017.
100. Tunçalp Ӧ et al., Quality of care for pregnant women and newborns—the WHO vision, BJOG, 2015, 122(8):1045–1049, doi:10.1111/1471-0528.13451.
101. UNFPA, State of the World’s Midwifery 2014, 2014, https://www.unfpa.org/sowmy.
102. Kohler H-P and Behrman JR, Benefits and costs of the population and demography targets for the post-2015 development agenda, in: Lomborg B, ed., Prioritizing Development, Cambridge: Cambridge University Press, 2018, pp. 375–398, doi:10.1017/9781108233767.023.
103. Miller G and Babiarz KS, Family planning program effects: evidence from microdata, Population and Development Review, 2016, 42(1):7–26, doi:10.1111/j.1728-4457.2016.00109.x.
104. Moreland S and Madsen EL, Demographic dividend models, in: Groth H and May JF, eds., Africa’s Population: In Search of a Demographic Dividend, Cham, Switzerland: Springer International Publishing, 2017, pp. 453–467, doi:10.1007/978-3-319-46889-1_28.
105. National Institute of Statistics of Rwanda, African Institute for Development Policy (AFIDEP) and UNFPA, Unlocking Rwanda’s Potential to Reap the Demographic Dividend, Nairobi: AFIDEP, 2017, https://www.afidep.org/publication/unlocking-rwandas-potential-to-reap-….
106. Drummond P, Thakoor V and Yu S, Africa rising: harnessing the demographic dividend, IMF Working Paper, Washington DC: International Monetary Fund, 2014, No. 14/143, http://elibrary.imf.org/view/IMF001/21549-9781498379878/21549-978149837….
107. Worldwatch Institute and Population Reference Bureau (PRB), Making the connection: population dynamics and climate compatible development, Fact Sheet, Washington, DC: PRB, 2014, https://www.prb.org//wp-content/uploads/2018/03/population-climate-brie….
108. Bongaarts J, Development: slow down population growth, Nature News, 2016, 530(7591):409, doi:10.1038/530409a.
109. Sexual and reproductive health and climate change, editorial, Lancet, 2009, 374(9694):949, doi:10.1016/S0140-6736(09)61643-3.
110. Bremner J, Patterson KP and Yavinsky R, Building resilience through family planning: a transformative approach for women, families and communities, Policy Brief, Washington, DC: PRB, 2015, https://www.prb.org/wp-content/uploads/2015/12/sahel-resilience-brief.p….
111. Shah IH, Santhya KG and Cleland J, Postpartum and post‐abortion contraception: from research to programs, Studies in Family Planning, 2015, 46(4):343–353, doi:10.1111/j.1728-4465.2015.00036.x.
112. Cleland J, Shah IH and Daniele M, Interventions to improve postpartum family planning in low‐ and middle‐income countries: program implications and research priorities, Studies in Family Planning, 2015, 46(4):423–441, doi:10.1111/j.1728-4465.2015.00041.x.
113. Schreiber CA et al., Ovulation resumption after medical abortion with mifepristone and misoprostol, Contraception, 2011, 84(3):230–233, doi:10.1016/j.contraception.2011.01.013.
114. WHO, Medical Eligibility Criteria for Contraceptive Use, fifth ed., 2015, http://www.who.int/reproductivehealth/publications/family_planning/Ex-S….
115. Huber D et al., Postabortion care: 20 years of strong evidence on emergency treatment, family planning, and other programming components, Global Health: Science and Practice, 2016, 4(3):481–494, doi:10.9745/GHSP-D-16-00052.
116. Yegon E et al., The quality of postabortion care in Tanzania: service provider perspectives and results from a service readiness assessment, Global Health: Science and Practice, 2019, 7(Suppl. 2):S315–S326, doi:10.9745/GHSP-D-19-00050.
117. Huber D, Postabortion care and the voluntary family planning component: expanding contraceptive choices and service options, Global Health: Science and Practice, 2019, 7(Suppl. 2):S207–S210, doi:10.9745/GHSP-D-19-00128.
118. Santhya KG and Jejeebhoy SJ, Sexual and reproductive health and rights of adolescent girls: evidence from low- and middle-income countries, Global Public Health, 2015, 10(2):189–221, doi:10.1080/17441692.2014.986169.
119. UNFPA, State of World Population 2016: 10, How Our Future Depends on a Girl at This Decisive Age, 2016, https://www.unfpa.org/sites/default/files/sowp/downloads/The_State_of_W….
120. UNFPA, State of World Population 2019: Unfinished Business, the Pursuit of Rights and Choices for ALL, 2019, https://www.unfpa.org/sites/default/files/pub-pdf/UNFPA_PUB_2019_EN_Sta….
121. Patton GC et al., Our future: a Lancet commission on adolescent health and wellbeing, Lancet, 2016, 387(10036):2423–2478, doi:10.1016/S0140-6736(16)00579-1.
122. Woog V and Kagesten A, The Sexual and Reproductive Health Needs of Very Young Adolescents Aged 10–14 in Developing Countries: What Does the Evidence Show?, New York: Guttmacher Institute, 2017, https://www.guttmacher.org/report/srh-needs-very-young-adolescents-in-d….
123. MacQuarrie KLD, Mallick L and Allen C, Sexual and reproductive health in early and later adolescence: DHS data on youth age 10–19, DHS Comparative Reports, Rockville, MD, USA: ICF, 2017, No. 45, https://dhsprogram.com/pubs/pdf/CR45/CR45.pdf.
124. UNICEF, Child Marriage: Latest Trends and Future Prospects, 2018, https://data.unicef.org/resources/child-marriage-latest-trends-and-futu….
125. UN Office of the High Commissioner on Human Rights, Convention on the rights of the child, 1989, https://www.ohchr.org/en/professionalinterest/pages/crc.aspx.
126. Langhaug LF, Sherr L and Cowan FM, How to improve the validity of sexual behaviour reporting: systematic review of questionnaire delivery modes in developing countries, Tropical Medicine & International Health, 2010, 15(3):362–381, doi:10.1111/j.1365-3156.2009.02464.x.
127. García-Moreno C et al., Global and Regional Estimates of Violence Against Women: Prevalence and Health Effects of Intimate Partner Violence and Non-Partner Sexual Violence, Geneva: WHO, 2013, https://www.who.int/reproductivehealth/publications/violence/9789241564….
128. Chandra-Mouli V et al., Contraception for adolescents in low and middle income countries: needs, barriers, and access, Reproductive Health, 2014, 11(1), doi:10.1186/1742-4755-11-1.
129. Kesterton AJ and Cabral de Mello M, Generating demand and community support for sexual and reproductive health services for young people: a review of the literature and programs, Reproductive Health, 2010, 7(1):25, doi:10.1186/1742-4755-7-25.
130. Denno DM, Hoopes AJ and Chandra-Mouli V, Effective strategies to provide adolescent sexual and reproductive health services and to increase demand and community support, Journal of Adolescent Health, 2015, 56(1):S22–S41, doi:10.1016/j.jadohealth.2014.09.012.
131. High Impact Practices in Family Planning, Adolescent-Friendly Contraceptive Services: Mainstreaming Adolescent-Friendly Elements into Existing Contraceptive Services, Washington, DC: USAID, 2015.
132. Population Division, UN Department of Economic and Social Affairs, Reproductive Health Policies 2017, Data Booklet, New York: UN, 2017, No. ST/ESA/ SER.A/396, https://www.un.org/en/development/desa/population/publications/pdf/poli….
133. WHO, WHO Consolidated Guideline on Self-Care Interventions for Health: Sexual and Reproductive Health and Rights, 2019.
134. Dunlop CL, Benova L and Campbell O, Effect of maternal age on facility-based delivery: analysis of first-order births in 34 countries of sub-Saharan Africa using demographic and health survey data, BMJ Open, 2018, 8(4):e020231–e020231, doi:10.1136/bmjopen-2017-020231.
135. Sheehan P et al., Building the foundations for sustainable development: a case for global investment in the capabilities of adolescents, Lancet, 2017, 390(10104):1792–1806, doi:10.1016/S0140-6736(17)30872-3.
136. Chalasani S et al., An investment case to guarantee the rights of adolescents, Journal of Adolescent Health, 2019, 65:S3–S7, doi:10.1016/j.jadohealth.2019.04.015.
137. UNFPA, Programme of Action of the International Conference on Population and Development, 20th Anniversary Edition, 2014, https://www.unfpa.org/sites/default/files/pub-pdf/programme_of_action_W….
138. Looker KJ et al., Global estimates of prevalent and incident herpes simplex virus type 2 Infections in 2012, PLOS ONE, 2015, 10(1):e114989, doi:10.1371/journal.pone.0114989.
139. de Sanjosé S et al., Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: a meta-analysis, Lancet Infectious Diseases, 2007, 7(7):453–459, doi:10.1016/S1473-3099(07)70158-5.
140. UNAIDS, Global HIV & AIDS statistics—2019, Fact Sheet, 2019, https://www.unaids.org/en/resources/fact-sheet.
141. WHO, Global Strategy for the Prevention and Control of Sexually Transmitted Infections: 2006–2015: Breaking the Chain of Transmission, 2007.
142. Korenromp EL et al., Global burden of maternal and congenital syphilis and associated adverse birth outcomes—estimates for 2016 and progress since 2012, PLOS ONE, 2019, 14(2):e0211720, doi:10.1371/journal.pone.0211720.
143. WHO, Human papillomavirus vaccines: WHO position paper, May 2017, Weekly Epidemiological Record, 2017, 19(92):241–268.
144. Storey A et al., Syphilis diagnosis and treatment during antenatal care: the potential catalytic impact of the dual HIV and syphilis rapid diagnostic test, comment, Lancet Global Health, 2019, 7(8):e1006–e1008, doi:https://doi.org/10.1016/S2214-109X(19)30248-7.
145. Ndowa F and Lusti-Narasimhan M, The threat of untreatable gonorrhoea: implications and consequences for reproductive and sexual morbidity, Reproductive Health Matters, 2012, 20(40):76–82, doi:10.1016/S0968-8080(12)40653-X.
146. Unemo M and Nicholas RA, Emergence of multidrug-resistant, extensively drug-resistant and untreatable gonorrhea, Future Microbiology, 2012, 7(12):1401–1422, doi:10.2217/fmb.12.117.
147. WHO, Vaccines in National Immunization Programme update 2019, 2019, https://www.who.int/docs/default-source/documents/immunization/data/vac….
148. WHO, WHO Recommendations on Newborn Health: Guidelines Approved by the WHO Guidelines Review Committee, 2017, https://apps.who.int/iris/bitstream/handle/10665/259269/WHO-MCA-17.07-e….
149. Newman L et al., Global estimates of syphilis in pregnancy and associated adverse outcomes: analysis of multinational antenatal surveillance data, PLOS Medicine, 2013, 10(2):e1001396, doi:10.1371/journal.pmed.1001396.
150. Tsu VD, Jeronimo J and Anderson BO, Why the time is right to tackle breast and cervical cancer in low-resource settings, Bulletin of the World Health Organization, 2013, 91(9):683–690, doi:10.2471/BLT.12.116020.
151. Ferlay J et al., Cancer Today, Database, Lyon, France: International Agency for Research on Cancer, 2018, https://publications.iarc.fr/Databases/Iarc-Cancerbases/Cancer-Today-Po….
152. WHO, Comprehensive Cervical Cancer Control: A Guide to Essential Practice, second ed., 2014, http://apps.who.int/iris/bitstream/10665/144785/1/9789241548953_eng.pdf….
153. Firnhaber C et al., Highly active antiretroviral therapy and cervical dysplasia in HIV-positive women in South Africa, Journal of the International AIDS Society, 2012, 15(2):17382–17382, doi:10.7448/IAS.15.2.17382.
154. WHO, WHO Guidelines for Screening and Treatment of Precancerous Lesions for Cervical Cancer Prevention, 2013, https://apps.who.int/iris/bitstream/handle/10665/94830/9789241548694_en….
155. Chido-Amajuoyi OG et al., A call for the introduction of gender-neutral HPV vaccination to national immunisation programmes in Africa, Lancet Global Health, 2019, 7(1):e20–e21, doi:10.1016/S2214-109X(18)30405-4.
156. Campos NG et al., The health and economic impact of scaling cervical cancer prevention in 50 low- and lower-middle-income countries, International Journal of Gynecology & Obstetrics, 2017, 138:47–56, doi:10.1002/ijgo.12184.
157. Clendinen C et al., Manufacturing costs of HPV vaccines for developing countries, Vaccine, 2016, 34(48):5984–5989, doi:10.1016/j.vaccine.2016.09.042.
158. WHO, Meeting of the strategic advisory group of experts on immunization, October 2018–conclusions and recommendations, Weekly Epidemiological Record, 2018, 93(49):661–680.
159. UNAIDS, Women and Girls and HIV, 2018, https://www.unaids.org/sites/default/files/media_asset/women_girls_hiv_….
160. UNAIDS and AIDSInfo, Number of new infections; population young women 15–24 and young men 15–24, 2018, data sheet, no date, http://aidsinfo.unaids.org/.
161. UNAIDS, 90-90-90: An Ambitious Treatment Target to Help End the AIDS Epidemic, 2014, https://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf.
162. WHO, Guideline on When to Start Antiretroviral Therapy and on Pre-Exposure Prophylaxis for HIV, 2015, https://apps.who.int/iris/bitstream/handle/10665/186275/9789241509565_e….
163. WHO, WHO expands recommendation on oral pre-exposure prophylaxis of HIV infection (PrEP), Policy Brief, 2015, https://apps.who.int/iris/bitstream/handle/10665/197906/WHO_HIV_2015.48….
164. Avert, Pre-exposure prophylaxis (PrEP) for HIV prevention, 2019, https://www.avert.org/professionals/hiv-programming/prevention/pre-expo….
165. Rodolph M, State of oral PrEP implementation and scale up, paper presented at Current State of Play: PrEP Implementation Update and Challenges, Madrid, Oct. 22, 2018, http://www.natap.org/2018/HIVR4P/HIVR4P_21.htm.
166. WHO, Consolidated Guideline on Sexual and Reproductive Health and Rights of Women Living with HIV, 2017, https://apps.who.int/iris/bitstream/handle/10665/254634/WHO-RHR-17.03-e….
167. Marston M, Zaba B and Eaton JW, Relative patterns of sexual activity and fertility among HIV positive and negative women—evidence from 46 DHS, PLOS ONE, 2018, 13(10):e0204584, doi:10.1371/journal.pone.0204584.
168. WHO, Web annex E: recommendations for use of hormonal contraception for women living with HIV using antiretroviral therapy, in: Updated recommendations on first-line and second-line antiretroviral regimens and post-exposure prophylaxis and recommendations on early infant diagnosis of HIV: interim guidelines, Supplement to the 2016 Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection, 2018, p. 10, https://apps.who.int/iris/handle/10665/276494.
169. Jewkes R et al., Factors associated with HIV sero-status in young rural South African women: connections between intimate partner violence and HIV, International Journal of Epidemiology, 2006, 35(6):1461–1468, doi:10.1093/ije/dyl218.
170. Jewkes R et al., Impact of exposure to intimate partner violence on CD4+ and CD8+ T cell decay in HIV infected women: longitudinal study, PLOS ONE, 2015, 10(3):e0122001, doi:10.1371/journal.pone.0122001.
171. Samuel M et al., Care of HIV-positive women aged 50 and over—can we do better?, International Journal of STD & AIDS, 2013, 25(4):303–305, doi:10.1177/0956462413504553.
172. Sundermann EE et al., Current challenges and solutions in research and clinical care of older persons living with HIV: findings presented at the 9th International Workshop on HIV and Aging, AIDS Research and Human Retroviruses, 2019, 35(11–12), doi:10.1089/aid.2019.0100.
173. Schnall R et al., In people living with HIV (PLWH), menopause (natural or surgical) contributes to the greater symptom burden in women: results from an online US survey, Menopause, 2018, 25(7):744–752, doi:10.1097/GME.0000000000001083.
174. Toorabally N et al., Association of HIV status with sexual function in women aged 45–60 in England: results from two national surveys, AIDS Care, 2020, 32(3):286–295, doi:10.1080/09540121.2019.1653436.
175. Dillon G et al., Mental and physical health and intimate partner violence against women: a review of the literature, International Journal of Family Medicine, 2013, doi:10.1155/2013/313909.
176. Ibrahim Z, Kuru-Utumpala J and Goulden J, Counting the Cost: The Price Society Pays for Violence Against Women, Geneva: CARE International, 2018, https://www.care-international.org/files/files/Counting_the_costofViole….
177. What Works to Prevent Violence, A Global Programme to Prevent Violence Against Women and Girls: A Summary of the Evidence, London: UK Aid, no date, https://www.whatworks.co.za/documents/publications/2-a-summary-of-the-e….
178. Jewkes R, What Works Evidence Review: Social Norms and Violence Against Women and Girls, London: What Works to Prevent Violence, 2017, https://www.whatworks.co.za/documents/publications/165-social-norms-evi….
179. Ellsberg M et al., Prevention of violence against women and girls: What does the evidence say?, Lancet, 2015, 385(9977):1555–1566, doi:10.1016/S0140-6736(14)61703-7.
180. Jewkes R et al., Effectiveness of Response Mechanisms to Prevent Violence Against Women and Girls: A Summary of the Evidence, London: What Works to Prevent Violence, 2014, https://www.whatworks.co.za/documents/publications/5-effectiveness-of-r….
181. Garcia-Moreno C et al., The health-systems response to violence against women, Lancet, 2014, 385(9977):1567–1579, doi:10.1016/S0140-6736(14)61837-7.
182. Hook C et al., Getting to Equal: Engaging Men and Boys in Sexual and Reproductive Health and Rights and Gender Equality, Washington, DC: Promundo-US, 2018, https://promundoglobal.org/resources/getting-equal-engaging-men-boys-se….
183. Remme M, Michaels-Igbokwe C and Watts C, Approaches to Assess Value for Money and Scale up of Violence Against Women and Girls Prevention: A Summary of the Evidence, London: What Works to Prevent Violence, 2014, https://www.whatworks.co.za/documents/publications/6-approaches-to-asse….
184. Ferrari G et al., Economic evaluation of public health interventions: an application to interventions for the prevention of violence against women and girls implemented by the "What Works to Prevent Violence Against Women and Girls?" global program, Journal of Interpersonal Violence, 2019, doi:10.1177/0886260519885118.
185. UNFPA, Costing the Three Transformative Results, 2019, https://www.unfpa.org/featured-publication/costing-three-transformative….
186. UN Women et al., Essential Services Package for Women and Girls Subject to Violence: Core Elements and Quality Guidelines, no date, http://www.unwomen.org/-/media/headquarters/attachments/sections/librar….
187. Ombelet W and Goossens J, Global reproductive health—Why do we persist in neglecting the undeniable problem of childlessness in resource-poor countries?, editorial, Facts, Views & Vision in ObGyn, 2017, 9(1):1–3.
188. Stellar C et al., A systematic review and narrative report of the relationship between infertility, subfertility, and intimate partner violence, International Journal of Gynecology and Obstetrics, 2016, 133(1):3–8, doi:10.1016/j.ijgo.2015.08.012.
189. Rouchou B, Consequences of infertility in developing countries, Perspectives in Public Health, 2013, 133(3):174–179, doi:10.1177/1757913912472415.
190. Rutstein S and Shah I, Infecundity, infertility, and childlessness in developing countries, DHS Comparative Reports, Calverton, MD, USA: ORC Macro and WHO, 2004, No. 9.
191. Dyer SJ and Patel M, The economic impact of infertility on women in developing countries—a systematic review, Facts, Views & Vision in ObGyn, 2012, 4(2):102–109.
192. Inhorn MC and Patrizio P, Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century, Human Reproduction Update, 2015, 21(4):411–426, doi:10.1093/humupd/dmv016.
193. Zegers-Hochschild F et al., International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009, Fertility and Sterility, 2009, 92(5):1520–1524, doi:10.1016/j.fertnstert.2009.09.009.
194. Boivin J et al., International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care, Human Reproduction, 2007, 22(6):1506–1512, doi:10.1093/humrep/dem046.
195. Hammarberg K et al., Improving access to ART in low-income settings through knowledge transfer: a case study from Zimbabwe, Human Reproduction Open, 2018, 2018:1–5, doi:10.1093/hropen/hoy017.
196. Mascarenhas MN et al., National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys, PLOS Medicine, 2012, 9(12):e1001356, doi:10.1371/journal.pmed.1001356.
197. Asemota OA and Klatsky P, Access to infertility care in the developing world: the family promotion gap, Seminars in Reproductive Medicine, 2015, 33(1):17–22, doi:10.1055/s-0034-1395274.
198. Kushnir VA and Lewis W, HIV/AIDS and infertility: emerging problems in the era of highly active antiretrovirals, Fertility and Sterility, 2011, 96(3):546–553, doi:10.1016/j.fertnstert.2011.05.094.
199. Stevenson EL, Hershberger PE and Bergh PA, Evidence-based care for couples with infertility, Journal of Obstetric, Gynecologic & Neonatal Nursing, 2016, 45(1):100–110, doi:10.1016/j.jogn.2015.10.006.
200. Teoh PJ and Maheshwari A, Low-cost in vitro fertilization: current insights, International Journal of Women’s Health, 2014, 6:817–827, doi:10.2147/IJWH.S51288.
201. Gerrits T et al., Infertility in the global south: raising awareness and generating insights for policy and practice, Facts, Views & Vision in ObGyn, 2017, 9(1):39–44.
202. UNHCR, Global Trends: Forced Displacement in 2018, 2018, https://www.unhcr.org/5d08d7ee7.pdf.
203. Women’s Refugee Commission, Save the Children et al., Adolescent Sexual and Reproductive Health Programs in Humanitarian Settings: An In-Depth Look at Family Planning Services, New York: Women’s Refugee Commission, Save the Children, UNHCR and UNFPA, 2012, https://www.unfpa.org/resources/adolescent-sexual-and-reproductive-heal….
204. McGinn T and Casey SE, Why don’t humanitarian organizations provide safe abortion services?, Conflict and Health, 2016, 10(8), doi:10.1186/s13031-016-0075-8.
205. Inter-Agency Working Group on Reproductive Health in Crises, Inter-Agency Field Manual on Reproductive Health in Humanitarian Settings, 2018, https://iawgfieldmanual.com/.
206. Casey SE et al., Progress and gaps in reproductive health services in three humanitarian settings: mixed-methods case studies, Conflict and Health, 2015, 9 (Suppl. 1):S3, doi:10.1186/1752-1505-9-S1-S3.
207. Chynoweth SK, Advancing reproductive health on the humanitarian agenda: the 2012–2014 global review, Conflict and Health, 2015, 9 (Suppl. 1):11, doi:10.1186/1752-1505-9-S1-I1.
208. Chynoweth SK, Freccero J and Touquet H, Sexual violence against men and boys in conflict and forced displacement: implications for the health sector, Reproductive Health Matters, 2017, 25(51):90–94, doi:10.1080/09688080.2017.1401895.
209. Tran N-T et al., Developing institutional capacity for reproductive health in humanitarian settings: a descriptive study, PLOS ONE, 2015, 10(9):e0137412, doi:10.1371/journal.pone.0137412.
210. Organisation for Economic Co-operation and Development (OECD), Service Delivery in Fragile Situations: Key Concepts, Findings and Lessons, 2008, https://www.oecd.org/dac/conflict-fragility-resilience/docs/40886707.pdf.
211. Krause S et al., Reproductive health services for Syrian refugees in Zaatri Camp and Irbid City, Hashemite Kingdom of Jordan: an evaluation of the Minimum Initial Services Package, Conflict and Health, 2015, 9(Suppl. 1):S4, doi:10.1186/1752-1505-9-S1-S4.
212. Blanchet K et al., Evidence on public health interventions in humanitarian crises, Lancet, 2017, 390(10109):2287–2296, doi:10.1016/S0140-6736(16)30768-1.
213. Jamison DT et al., Universal health coverage and intersectoral action for health: key messages from Disease Control Priorities, 3rd edition, Lancet, 2018, 391(10125):1108–1120, doi:10.1016/S0140-6736(17)32906-9.
214. Chang AY et al., Past, present, and future of global health financing: a review of development assistance, government, out-of-pocket, and other private spending on health for 195 countries, 1995–2050, Lancet, 2019, 393(10187):2233–2260, doi:10.1016/S0140-6736(19)30841-4.
215. WHO, WHO Global Health Expenditure Database, 2020, http://apps.who.int/nha/database/Regional_Averages/Index/en.
216. Waddington C and Sambo C, Financing health care for adolescents: a necessary part of universal health coverage, Bulletin of the World Health Organization, 2015, 93:57–59, doi:10.2471/BLT.14.139741.
217. Dieleman JL, Micah AE and Murray CJL, Global health spending and development assistance for health, JAMA, 2019, 321(21):2073–2074, doi:10.1001/jama.2019.3687.
218. WHO, Universal health coverage (UHC), Fact Sheet, no date, https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc).
Suggested Citation
Sully EA et al., Adding It Up: Investing in Sexual and Reproductive Health 2019, New York: Guttmacher Institute, 2020, http://www.guttmacher.org/report/adding-it-up-investing-in-sexual-repro….
Acknowledgments
This report was written by Elizabeth A. Sully, Ann Biddlecom, Jacqueline E. Darroch, Taylor Riley, Naomi Lince-Deroche, Lauren Firestein and Rachel Murro, all of the Guttmacher Institute, and Lori S. Ashford, of Clarity Global Health. Haley Ball, of the Guttmacher Institute, edited the report.
The authors thank Eva Weissman, independent consultant, for her contributions on interventions and for evaluating and compiling direct cost data. They also acknowledge the following Guttmacher colleagues (in alphabetical order): Suzette Audam, for data compilation and processing; Jonathan Bearak, Cynthia Beavin and Anna Popinchalk, for abortion and unintended pregnancy estimates; Heather Boonstra, Alanna Galati, Sophia Sadinsky and Susheela Singh, for providing input and reviewing drafts; Marielle Kirstein, for research assistance; Onikepe Owolabi, for her guidance and medical expertise on treatment assumptions; and Emily Swanson, for coordination of external reviews, editing and production. We also thank the following colleagues for inputs they made when they were affiliated with the Guttmacher Institute: Adesegun Fatusi, Anqa Khan, Grant Kopplin, Lorraine Kwok and Colette Rose.
We thank Eman Aboaldahab ElSayed, independent consultant, for data processing; Vladimíra Kantorová, Population Division, United Nations Department of Economic and Social Affairs, for guidance on country-specific estimates of family planning indicators; John Stover, Avenir Health, for guidance on data and estimation from the Spectrum AIM model; and Doris Chou, World Health Organization (WHO), for specialized tabulations of maternal mortality estimates.
In addition, the authors are grateful for the suggestions and advice offered by the following colleagues who reviewed the manuscript: Howard Friedman and Yann Lacayo, United Nations Population Fund (UNFPA); Venkatraman Chandra-Mouli, Karin Stenberg and Melanie Taylor, WHO; Fila Magnus and Victoria Watson, International Youth Alliance for Family Planning; Michael Mbizvo and John Townsend, Population Council; Jason Bremner, Family Planning 2020; Beth Fredrick, Johns Hopkins University; Supriya Madhavan, World Bank; Meggie Mwoka, African Population and Health Research Center; Rose Oronje, African Institute for Development Policy; Souvik Pyne, The YP Foundation; Jonathan Rucks, Population Action International; Suzanne Serruya, Pan American Health Organization; John Skibiak, Reproductive Health Supplies Coalition; Ellen Starbird, U.S. Agency for International Development; and Michelle Weinberger, Avenir Health.
This report was made possible by UK Aid from the UK Government and grants from the Bill & Melinda Gates Foundation, The Children’s Investment Fund Foundation, the Dutch Ministry of Foreign Affairs and UNFPA. The findings and conclusions contained within are those of the authors and do not necessarily reflect positions or policies of the donors. The Guttmacher Institute gratefully acknowledges the unrestricted funding it receives from many individuals and foundations—including major grants from the William and Flora Hewlett Foundation and the David and Lucile Packard Foundation—which undergirds all of the Institute’s work.
American Samoa, Dominica, Marshall Islands, Nauru and Tuvalu. Following UN Population Division classifications, Kosovo is collapsed with Serbia for all calculations. Use of the 30-day cut-off produces minimum estimates of the number of women wanting to avoid pregnancy and the need for contraception. Other definitions of “current” sexual activity (e.g., sex in the last three months, last year or ever) result in larger proportions of unmarried women classified as sexually active. This report uses the revised 2017 WHO definition of abortion safety.25 Safe abortions are those that use a WHO-recommended method appropriate to the pregnancy duration and are done by a trained provider. Less safe abortions meet only one of these criteria, and least safe abortions meet neither criterion. We use “unsafe” to refer to both less safe and least safe abortions. Defined as fetal deaths before 28 weeks’ gestation.30 Defined as babies born with no signs of life at or after 28 weeks’ gestation.30 All cost estimates in this report are one-year estimates in 2019 U.S. dollars. Oral contraceptive pill, injectable, patch, ring and emergency contraception. Because this report focuses on maternal and newborn health during pregnancy and for approximately six weeks after birth, it excludes the cost of antiretroviral therapy for women who were receiving it prior to pregnancy, even if they continue to receive it while pregnant and postpartum. This report also excludes antiretroviral therapy costs for women beyond six weeks postpartum and for infants older than six weeks. Country-level data were used for Bangladesh,26 Ethiopia,27 India28 and Nepal.29 Use of the 30-day cut-off produces minimum estimates of the number of women wanting to avoid pregnancy and the need for contraception. Other definitions of “current” sexual activity (e.g., sex in the last three months, last year or ever) result in larger proportions of unmarried women classified as sexually active.
Additional Downloads
- Appendix Tables: Estimates for groupings of low- and middle-income countries adding-it-up-2019-report-appendix-tables.xlsx