Background
This report presents new state-level estimates of contraceptive prevalence among women of reproductive age in the United States. While surveillance efforts such as the National Survey of Family Growth (NSFG) and the National Health and Nutrition Examination Survey (NHANES) collect nationally representative data on reproductive health measures, the Behavioral Risk Factor Surveillance System (BRFSS) offers an opportunity to explore basic indicators of reproductive health among resident women in each state. In particular, BRFSS data show state-by-state differences in contraceptive use. The estimates for 2017 presented here provide the most comprehensive documentation of contraceptive use at the state level since 2004.
Data and Methods
The BRFSS is a surveillance system that conducts monthly cross-sectional surveys in all 50 states, the District of Columbia and three U.S. territories (Guam, Puerto Rico and the U.S. Virgin Islands). Landline and cellphone interviews are used to collect retrospective self-reported data from adult men and women aged 18 and older. Data collection is conducted separately by each jurisdiction, using complex sampling designs determined by that jurisdiction and reviewed by the Centers for Disease Control and Prevention (CDC). The BRFSS questionnaire consists of three components: a core set of questions used by all jurisdictions that covers demographics, current health conditions and health-related behaviors; optional modules on specific health topics (e.g., sexual and reproductive health, cardiovascular disease, arthritis); and questions jurisdictions have developed for their own use. The questions from the core and optional modules are edited and evaluated by the CDC; questions added by individual jurisdictions are not.1 More detailed information on questionnaires, survey methodology, sample design, response rates, fieldwork procedures and variance estimation is published elsewhere.2,3 Data, representative of noninstitutionalized adult residents of each state with available data, are publicly available for download on the BRFSS website.4
The tables in this report present basic tabulations of contraceptive method use data from the 2017 BRFSS. In 2017, key questions regarding women’s reproductive health were asked in the optional Preconception Health/Family Planning module. Forty-three jurisdictions included this optional module among their survey questions.* Our analytic sample is limited to female respondents aged 18–49 (n=61,306) who were living in 40 of these 43 jurisdictions. Illinois and Kentucky were excluded because they did not collect data for the entirety of 2017; the U.S. Virgin Islands were excluded because of a low number of observations. In addition, estimates for the District of Columbia and Puerto Rico are included in the report’s tables, but excluded from highlighted state comparisons.
All analyses were performed using Stata version 15.1. We applied sampling weights that yield estimates representative of resident women aged 18–49 within each state or territory to account for the BRFSS’s multistage, probability-based complex sample design. In addition, we used design variables for the sampling stratum and cluster to obtain correct standard errors for all estimates.
Weighted estimates were calculated to determine the proportion of women who reported using contraceptives at last sex among all women and among women at risk of unintended pregnancy. Women were categorized as at risk of unintended pregnancy at the time of the interview if they reported they were currently sexually active with one or more male partners, were not currently pregnant or trying to become pregnant, and had not had a hysterectomy.† The survey questions used for this analysis came from both the core survey and the optional module, and the specific questions and the answer choices provided to survey respondents are shown in the appendix. Of note, contraceptive method distributions presented here indicate the most effective methods used at last sex (referred to subsequently in this report as the “primary” method), as only the most effective method residents reported as having used at last sex was recorded in the BRFSS questionnaire.‡ Contraceptive methods were classified, according to first-year typical-use failure rates, into the following categories: permanent, long-acting reversible, moderately effective and least effective.§ 5,6 The contraceptive effectiveness classifications used in this report align with designations used by the CDC.7
Women at risk of unintended pregnancy who did not specify the type of contraceptive they used were included in estimates of overall contraceptive use but excluded from estimates where contraceptive use is grouped by the effectiveness of the method used. Estimates that did not meet reliability standards established for BRFSS by the CDC have been suppressed (i.e., a relative standard error greater than 30% or an unweighted denominator of fewer than 50 respondents).8 Estimates for certain methods did not meet the criteria for reliability in some jurisdictions and were therefore further grouped with other methods in their respective contraceptive effectiveness classifications: injectables, patches and rings were grouped together under “other non-LARC hormonal,” and emergency contraception, diaphragms, cervical rings, cervical caps, rhythm method, natural family planning and spermicidal methods were grouped together under “other.”
Highlighted Findings
Contraceptive use by risk of unintended pregnancy
- Across the 38 states with available data, the majority of all resident women aged 18–49 reported having used one or more contraceptive methods the last time they had sex with a partner, ranging from 62% in Hawaii to 78% in Oregon and Maine (Table 1).
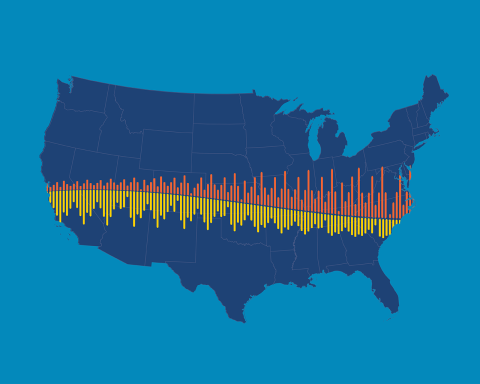
- Among women at risk of unintended pregnancy, contraceptive use ranged from 66% in Delaware to 84% in Maine (Figure 1).
- Use of contraceptive methods was somewhat higher among women living in the West and Northeast regions of the United States, as compared with use among women living in the South and Midwest.
Contraceptive use among women at risk of unintended pregnancy
- The proportion of women at risk of unintended pregnancy who report use of highly effective long-acting reversible contraceptive (LARC) methods ranges from 6% in Alabama to 27% in Maine (Table 2).
- The distribution of specific contraceptive methods used by women at risk of unintended pregnancy varies widely across states (Table 3).
- Nationally, female sterilization is the second most commonly used form of contraception (not shown); however, use differs considerably by state, ranging from 7% in Connecticut to 27% in West Virginia.
- There is also wide variation in IUD use among women at risk of unintended pregnancy, ranging from 5% in Louisiana and Alaska to 24% in Maine.
- Among states with available data, implant use is highest in New Mexico (8%).
- Birth control pills are one of the most commonly used primary methods of contraception, ranging from 11% in Alaska to 27% in Massachusetts.
- Condoms remain a popular form of primary birth control in all states with available data, ranging from 10% in West Virginia to 25% in Alaska and New York.
Discussion
Individuals use contraceptives to prevent unwanted pregnancies. Nationally, among U.S. women at risk of unintended pregnancy, the proportion who use a contraceptive method increased from 78% in 1982 to 89% in 2008 and has stayed at approximately that level for the past decade.8–10 More than six million women received publicly funded contraceptive services in 2015; this national effort helped women avoid an estimated 1.86 million unintended pregnancies, including 876,100 unplanned births and 628,600 abortions.11
Estimates presented here highlight differences in the most effective contraceptive method used at last sex among resident women aged 18–49 across the United States—both among this age-group overall and among the subgroup at risk of unintended pregnancy. In every state, the majority of women of reproductive age are using some form of contraceptive, and the rate of use is higher among women at risk of unintended pregnancy than among all women of reproductive age. Use estimates for primary methods show wide variability across the states, especially for female sterilization, IUDs, oral contraceptives and condoms. Maine has the highest levels of contraceptive use among women at risk of unintended pregnancy, driven by comparatively high use of LARCs and moderately effective methods, and comparatively low use of the least effective methods.
The state-level BRFSS and national NSFG differ in some significant ways that prevent direct comparison of contraceptive use estimates. First, the NSFG asks about method use among respondents aged 15–44, while the BRFSS asks about method use among respondents aged 18–49. A supplemental analysis of these 2017 BRFSS data in which we narrowed the sample to those aged 18–44 yielded higher contraceptive use prevalence across jurisdictions (not shown), as compared with the contraceptive use prevalence presented in this report among the full sample aged 18–49. In addition, the primary question addressing current contraceptive use in the NSFG asks about use in the interview month, while the BRFSS item asks about use at last sex. Finally, respondents to the NSFG and the BRFSS are not asked about their experience of hysterectomy in the same manner: All NSFG respondents who are currently not pregnant are asked if they ever had a hysterectomy; in the BRFSS, only nonusers of contraceptives are asked about hysterectomy as a possible reason for nonuse (see Additional Notes on the Data for more information). Given these key differences between the national and state-level data, we advise against making direct comparisons between the two data sources.
This report highlights wide variation in women’s contraceptive use across the United States and points to the need for ongoing systematic collection of subnational data, and we encourage further research to investigate differences in women’s contraceptive use at the state level by individual and context-related characteristics.
Additional Notes on the Data
- Concurrent use of multiple methods cannot be ascertained with these data. There is a growing body of literature that indicates some individuals employ contraceptive strategies that are more complex than using a single method at each coital act, and several studies suggest that less effective methods are more commonly used than was previously detected.12–16 Therefore, BRFSS data likely underestimate the use of methods, such as condoms and withdrawal, that are often employed concurrently by dual method users. The BRFSS uses an open-ended question to determine what method respondents used at last sex, and responses are probed only if clarification is necessary (e.g., to determine whether an IUD user uses a hormonal or nonhormonal IUD). Studies have shown that many women in the United States underreport their use of least effective methods when not prompted with an exhaustive list of options.8
- BRFSS respondents who had had a hysterectomy could only be identified if they cited this as a reason for not using a birth control method the last time they had sex. Therefore, respondents reporting a hysterectomy in this data set were excluded from the denominator of women at risk of unintended pregnancy used to calculate method-specific contraceptive prevalence. By not fully identifying the population of women aged 18–49 who have had a hysterectomy, we may be inflating the number of women at risk of unintended pregnancy by falsely categorizing them into this group. Inflating the number of women at risk may, in turn, underestimate the proportion of contraceptive users among women at risk of unintended pregnancy.
- We defined women as being at risk of unintended pregnancy if they cited “don’t care if [I] get pregnant” as a reason for contraceptive nonuse. We consider women expressing this uncertainty about pregnancy in the short term as at risk of unintended pregnancy because evidence indicates that some women report both ambivalent/indifferent pregnancy attitudes and desires to avoid pregnancy; that is, these are not mutually exclusive categories.17–19 The CDC, on the other hand, categorizes ambivalent women as not at risk of unintended pregnancy in its most recent analyses of BRFSS data.7 Among women who did not use contraceptives at last sex, the proportion citing “don’t care if [I] get pregnant” ranged from 2% in Louisiana to 9% in New York (not shown).
- Questions in the 2017 BRFSS on current use of birth control focus on “the last time” respondents had sex: “Did you or your partner do anything the last time you had sex to keep you from getting pregnant?” This differs from earlier BRFSS rounds that had asked what respondents or their partner were doing “now” to prevent pregnancy.
- Information on contraceptive use was self-reported and may be subject to recall or social desirability biases. Nonresponse bias is likely minimized in these data, as the weighting methodology used by BRFSS adjusts for this possibility.
FOOTNOTES
*Alabama, Alaska, Arizona, California, Connecticut, Delaware, District of Columbia, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Minnesota, Mississippi, Missouri, Nebraska, Nevada, New Jersey, New Mexico, New York, North Carolina, Ohio, Oklahoma, Oregon, Pennsylvania, Puerto Rico, South Carolina, South Dakota, Texas, U.S. Virgin Islands, Utah, Virginia, West Virginia, Wisconsin and Wyoming.
†Women who answered “don’t care if [I] get pregnant” when asked about their rationale for nonuse were considered in this report to be at risk of unintended pregnancy (see Additional Notes on the Data for more information).
‡Because the use of more than one method was not recorded in the BRFSS, use of less effective contraceptive methods was likely underestimated.
§Permanent methods: female sterilization or male sterilization, as reported by respondent. Long-acting reversible contraceptive (LARC) methods: IUDs and contraceptive implants. Moderately effective methods: injectables, pills, patches and vaginal rings. Least effective methods: male and female condoms, diaphragm, cervical cap, sponge, rhythm method, natural family planning, withdrawal, spermicidal foam/jelly/film/cream and emergency contraception.
Appendix
BRFSS survey questions relevant to this analysis
REFERENCES
1. U.S. Department of Health and Human Services (HHS), Healthy People.gov: behavioral risk factor surveillance system, no date, https://www.healthypeople.gov/2020/data-source/behavioral-risk-factor-surveillance-system.
2. Centers for Disease Control and Prevention (CDC), The BRFSS Data User Guide, 2013, https://www.cdc.gov/brfss/data_documentation/pdf/UserguideJune2013.pdf.
3. CDC, Behavioral Risk Factor Surveillance System: Overview BRFSS 2016, 2017, https://www.cdc.gov/brfss/annual_data/2016/pdf/overview_2016.pdf.
4. CDC, BRFSS Annual Survey Data, 2018, https://www.cdc.gov/brfss/annual_data/annual_data.htm.
5. Trussell J, Contraceptive failure in the United States, Contraception, 2011, 83(5):397–404.
6. HHS, Effectiveness of family planning methods, no date.
7. Pazol K et al., Contraceptive use among women at risk for unintended pregnancy in the context of public health emergencies—United States, 2016, Morbidity and Mortality Weekly Report, 2018, 67(32):898–902.
8. Jones J, Mosher W and Daniels K, Current contraceptive use in the United States, 2006–2010, and changes in patterns of use since 1995, National Health Statistics Reports, 2012, 18(60):1–25.
9. Mosher W and Bachrach C, Contraceptive Use, United States, 1980, Washington, DC: Government Printing Office, 1986.
10. Kavanaugh ML and Jerman J, Contraceptive method use in the United States: trends and characteristics between 2008, 2012 and 2014, Contraception, 2018, 97(1):14–21.
11. Frost JJ et al., Publicly Funded Contraceptive Services at U.S. Clinics, 2015, New York: Guttmacher Institute, 2017, https://www.guttmacher.org/report/publicly-funded-contraceptive-services-us-clinics-2015.
12. Frohwirth L et al., The complexity of multiple contraceptive method use and the anxiety that informs it: implications for theory and practice, Archives of Sexual Behavior, 2016, 45(8):2123–2135.
13. Brown J et al., Multiple method contraception use among African American adolescents in four US cities, Infectious Diseases in Obstetrics and Gynecology, 2011, http://dx.doi.org/10.1155/2011/765917.
14. Frost JJ, Singh S and Finer LB, U.S. women’s one-year contraceptive use patterns, 2004, Perspectives on Sexual and Reproductive Health, 2007, 39(1):48–55.
15. Jones RK, Lindberg LD and Higgins JA, Pull and pray or extra protection? Contraceptive strategies involving withdrawal among US adult women, Contraception, 2014, 90(4):416–421.
16. Whittaker PG et al., Withdrawal attitudes and experiences: a qualitative perspective among young urban adults, Perspectives on Sexual and Reproductive Health, 2010, 42(2):102–109.
17. Aiken ARA et al., Rethinking the pregnancy planning paradigm: unintended conceptions or unrepresentative concepts?, Perspectives on Sexual and Reproductive Health, 2016, 48(3):147–151, https://doi.org/10.1363/48e10316.
18. Miller WB, Barber JS and Gatny HH, The effects of ambivalent fertility desires on pregnancy risk in young women in the USA, Population Studies, 2013, 67(1):25–38.
19. Yoo SH, Guzzo KB and Hayford SR, Understanding the complexity of ambivalence toward pregnancy: Does it predict inconsistent use of contraception?, Biodemography and Social Biology, 2014, 60(1):49–66.