- Publicly supported family planning clinics play a crucial role in the health care system, providing essential contraceptive services to millions of people every year.
- These safety-net clinics have faced several obstacles since 2015, such as the Title X domestic gag rule, the COVID-19 pandemic and the overturning of Roe v. Wade.
- The proportion of clinics offering a wide range of contraceptive services on-site has remained relatively stable since 2015. However, provision of implants has increased, while the number of clinics offering fertility awareness–based methods and emergency contraceptive pills has decreased.
- The use of telemedicine to dispense oral contraceptive pills rose dramatically from 2015 to 2022–2023, likely driven by an increased use of telemedicine that began during the COVID-19 pandemic.
- The use of several protocols that support patient access to contraceptives has increased, including prescribing at least 12 months of oral contraceptive pills at the initial visit, offering both pills and refills on-site, dispensing oral contraceptive pills using the Quick Start protocol and offering advanced provision of emergency contraception, especially among Planned Parenthood clinics.
- The availability of general health and other sexual and reproductive health services in these clinics has also remained largely stable, although availability of HIV pre-exposure prophylaxis and mental health screening has increased notably since 2015.
Publicly Supported Family Planning Clinics in 2022–2023: Trends in Service Delivery Practices and Protocols
Author(s)
, , , andReproductive rights are under attack. Will you help us fight back with facts?
Key Points
Background
Publicly supported family planning clinics have weathered intense upheaval in recent years, from the disruption to the Title X network wrought by the Trump administration’s “domestic gag rule” to the COVID-19 pandemic, followed by the ripple effects of the Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization. Despite these challenges, these sites have continued to serve as a vital source of sexual and reproductive health (SRH) care, providing widespread availability of a range of contraceptive methods and increasing availability of patient-centered contraceptive dispensing protocols. These clinics are particularly important because a large proportion of their patients come from marginalized communities.
Publicly supported family planning clinics is a category made up of several types of clinics: Planned Parenthood clinics, federally qualified health clinics (FQHCs), public health department clinics, hospital clinics and other independent clinics. Among these, this study finds, Planned Parenthood facilities offer the broadest range of contraceptive options and the widest availability of protocols supporting patient access to contraception, despite bearing the brunt of political attacks targeting reproductive health care. In addition, health departments have made markable strides toward increasing patient-centered contraceptive care, performing as well or better than FQHCs on most measures.
Understanding the range of services provided by these clinics and how these services have changed since 2015 provides data necessary for development of evidence-based policies that ensure access to essential health services, especially as sexual and reproductive health provision is increasingly affected by policy restrictions. In addition, comparing service provision across clinic types allows for the identification of successes achieved by and challenges for the nation’s safety-net family planning clinics.
Publicly supported clinics that offer contraceptive services provide essential health care for millions of people in the United States every year. There are more than 10,000 sites that are considered publicly supported clinics in the United States.1 These clinics offer contraceptive services to the public and use public funding, including federal, state or local funding through programs like Medicaid or Title X, to provide free or reduced-fee services to eligible patients.2
Some publicly supported clinics are administered independently, but most are linked to larger national, state, or county organizations or agencies. In 2015, FQHCs accounted for 54% of clinics providing publicly supported contraceptive services, health departments accounted for 21%, other independent clinics accounted for 10%, hospital outpatient clinics accounted for 8%, and Planned Parenthood clinics accounted for 6%.* However, in terms of patients served, Planned Parenthood clinics served 32% of all female contraceptive patients, while FQHCs served 30%, health departments served 20%, hospital outpatient clinics served 10% and other clinics served 8%.1
Of the roughly 25 million women† who receive contraceptive care each year,3 18% receive this care from publicly supported clinics.4 In particular, low-income, uninsured and young women rely on these clinics for contraceptive services. Immigrant women and women of color also receive care from these clinics at higher proportions than their counterparts.4
Publicly supported clinics provide contraceptive services such as contraceptive method counseling, provision, prescriptions and check-ups. In addition to offering contraceptive services, many of these sites also provide critical SRH services, including Pap tests, pelvic exams, STI testing and treatment, and pregnancy tests. Most women who visit a publicly supported clinic for contraceptive or SRH services report that this site was their usual source of medical care (65%).4
The Guttmacher Institute collected data from a sample of publicly supported family planning sites in 2015, after the implementation of the Affordable Care Act (ACA). That study found that long-acting reversible contraceptives (LARCs) were becoming more widely available at these publicly supported sites. In addition, publicly supported family planning clinics were providing many noncontraceptive services; for example, primary care was provided at more than half of the sampled sites.4
However, the publicly funded family planning clinic network has experienced much disruption since that time. Restrictions to the federal Title X family planning program, which helps fund many publicly supported clinics, were enacted by the Trump administration in 2019, prohibiting Title X recipients from making abortion referrals and imposing financial and physical separation requirements for sites offering abortion care, among other restrictions.5
As a result of these domestic gag rule restrictions, approximately 1,000 clinics left the Title X program and only 1.5 million patients were served in 2020, compared with four million in 2018.6 In addition, this time period coincided with the start of the COVID-19 pandemic, which also affected contraceptive service provision.7,8 Researchers have estimated that approximately two-thirds of the decline in patients served by Title X was a result of the changes to the program made by the Trump administration and approximately one-third was a result of COVID-19.9
The Biden administration rescinded the Title X restrictions in 2021, and some sites that left Title X as a result of the gag rule have since rejoined, although the effects of the restrictions still linger.10,11 In addition, as vaccines and treatments became widely available, the impact of the COVID-19 pandemic on contraceptive service provision waned.12 More recently, in 2022, the Supreme Court’s Dobbs decision overturned Roe v. Wade, which led to an increase in abortion restrictions and bans in many states. Although a small proportion of family planning clinics are abortion providers (in 2015, 4% offered procedural abortions and 8% medication abortions),4 many family planning clinics provide abortion-related care such as pregnancy testing, referrals for abortion care and nondirective options counseling.
Methodology
Between November 2022 and December 2023, we surveyed a nationally representative sample of 2,146 clinics providing publicly supported contraceptive services. Our sample was stratified by Title X status (received Title X funding or did not) and clinic type (FQHCs, Planned Parenthood clinics, health departments, and hospitals and other sites). We programmed and hosted the online survey using Qualtrics. Respondents were eligible if they were family planning directors or administrators at publicly supported clinics providing family planning services in 2022.
We present results on key characteristics of clinics and variation in service offerings and provision protocols. We provide breakdowns by clinic type (health department, Planned Parenthood, FQHCs, hospital and other) and service focus (reproductive health, and primary care and other). We also compare findings from the 2022–2023 survey to those from 2015, when Guttmacher last conducted a survey of clinics providing contraceptive services. The key measures we report on in this report include clinic characteristics, such as number of patients served and clinic hours; clinic finances, such as receipt of Title X funding; contraceptive methods provided; sexual and reproductive health services provided; and contraceptive dispensing protocols.
A total of 446 clinics completed the survey, corresponding to an overall response rate of 24%, which is lower than the 50% response rate in 2015 (sample N=1,839; analytic sample=867). All cases were weighted for sampling ratios and nonresponse, and the results presented are nationally representative. All comparisons mentioned in the text are statistically significant at the p<.05 level unless otherwise indicated, although some significant comparisons are not mentioned in the report. See additional information about the survey, sample and methods of analysis in the Methodology Appendix.
Clinic Characteristics
Clinic focus
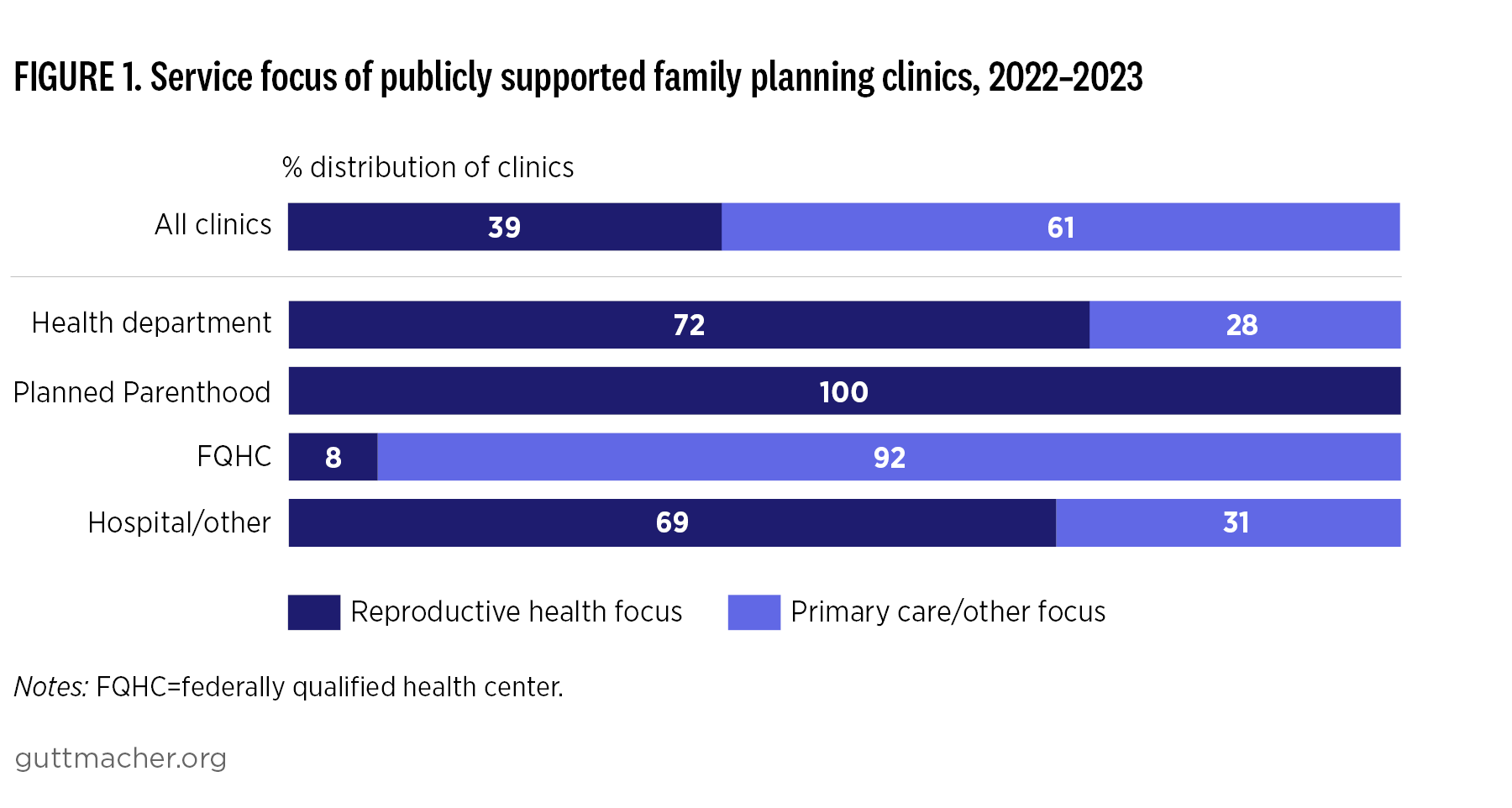
Nearly four in 10 publicly supported family planning clinics in 2022–2023 reported their principal service focus as specialized reproductive health care, meaning they primarily offer contraceptive and related SRH services. This is roughly the same proportion as in 2015 (Appendix Table 1).
- More than two-thirds of health department clinics and hospital and other clinics, and all Planned Parenthood clinics, reported a service focus on reproductive health, compared with 8% of FQHCs (Figure 1). There was an increase from 2015 among hospital and other clinics, when just more than half of these clinic types reported a reproductive health service focus.
Patient caseload
More than one-third of clinics reported that 50% or more of the patients they serve receive contraceptive services; this has remained consistent since 2015.
- Compared with the proportion in 2015, the proportion of patients in 2022–2023 receiving contraceptive services decreased at Planned Parenthood facilities and increased at hospital and other clinic types.
- FQHCs reported a much smaller proportion of patients receiving contraceptive services compared with other clinic types, as 33% of facilities reported fewer than 10% of patients receiving those services.
Slightly more than half of clinics reported serving fewer than 20 contraceptive patients per week (Appendix Table 1). A quarter of clinics reported serving 20–49 patients per week, and about a fifth served 50 or more.
- Compared with 2015 data, the contraceptive caseload in 2022–2023 among health departments and Planned Parenthood clinics decreased.
- Contraceptive patient caseload varied dramatically by clinic type: Planned Parenthood facilities served many more contraceptive patients per week and health departments reported fewer, compared with the number of patients served at the other clinic types.
Scheduling
Overall, there has not been a change in the availability of extended office hours for contraceptive care between 2015 and 2022–2023. However, the proportion of health departments offering extended office hours decreased from 18% in 2015 to 3% in 2022–2023.
- In addition, there was variation in the availability of extended hours between clinic types in 2022–2023. While 42% of clinics overall offered extended hours, more than two-thirds of Planned Parenthood clinics and more than half of FQHCs reported doing so.
One in four publicly supported family planning clinics reported offering same-day appointments for contraceptive care—a decline from 52% in 2015 to 25% in 2022–2023 (Appendix Table 1).
- FQHCs, as well as hospital and other clinic types, report the highest availability of same-day appointments in our sample (28% and 33%, respectively). However, all clinic types saw a decrease in same-day appointment availability in 2022–2023 when compared with the same-day availability in 2015. Planned Parenthood clinics experienced the greatest drop, to just 15% from 62% in 2015.
The average number of hours publicly funded family planning clinics provide contraceptive services per week remained relatively unchanged from 2015 to 2022–2023; there were no differences between years by clinic type.
- FQHCs report providing the highest average number of weekly hours for contraceptive care provision, at an average of 43 hours per week.
Overall, patient wait time for an initial contraceptive care visit has doubled since 2015, from an average of three days to six days.
- Planned Parenthood clinics have experienced the largest increase in wait times (from one day to six days).
Health insurance and clinic revenue
Clinic respondents in 2022–2023 reported that about 60% of patients paid for their contraceptive care using public insurance; this did not change from 2015 (data not shown).
- However, the proportion of patients using private insurance increased between 2015 and 2022–2023 from 15% to 19%, while the proportion of patients that did not use either public or private insurance decreased from 28% to 21%. These changes were driven by shifts in health insurance status among patients served by health departments and Planned Parenthood facilities.
In the 2022–2023 survey, 44% of clinics reported any decline to the clinic’s annual revenue since 2018 (data not shown). Respondents could report multiple reasons for the decline in revenue.
- The largest proportion of clinics reported decreased revenue from COVID-related patient declines (37%), followed by decreased revenue from patient fees (20%), cuts in federal funding (14%), decreased revenue from Medicaid reimbursement (14%), decreased revenue from private insurance reimbursement (10%), and cuts in state or local funding (10%).
On-site Provision of Contraceptive and Other Health Services
Trends in contraceptive method availability
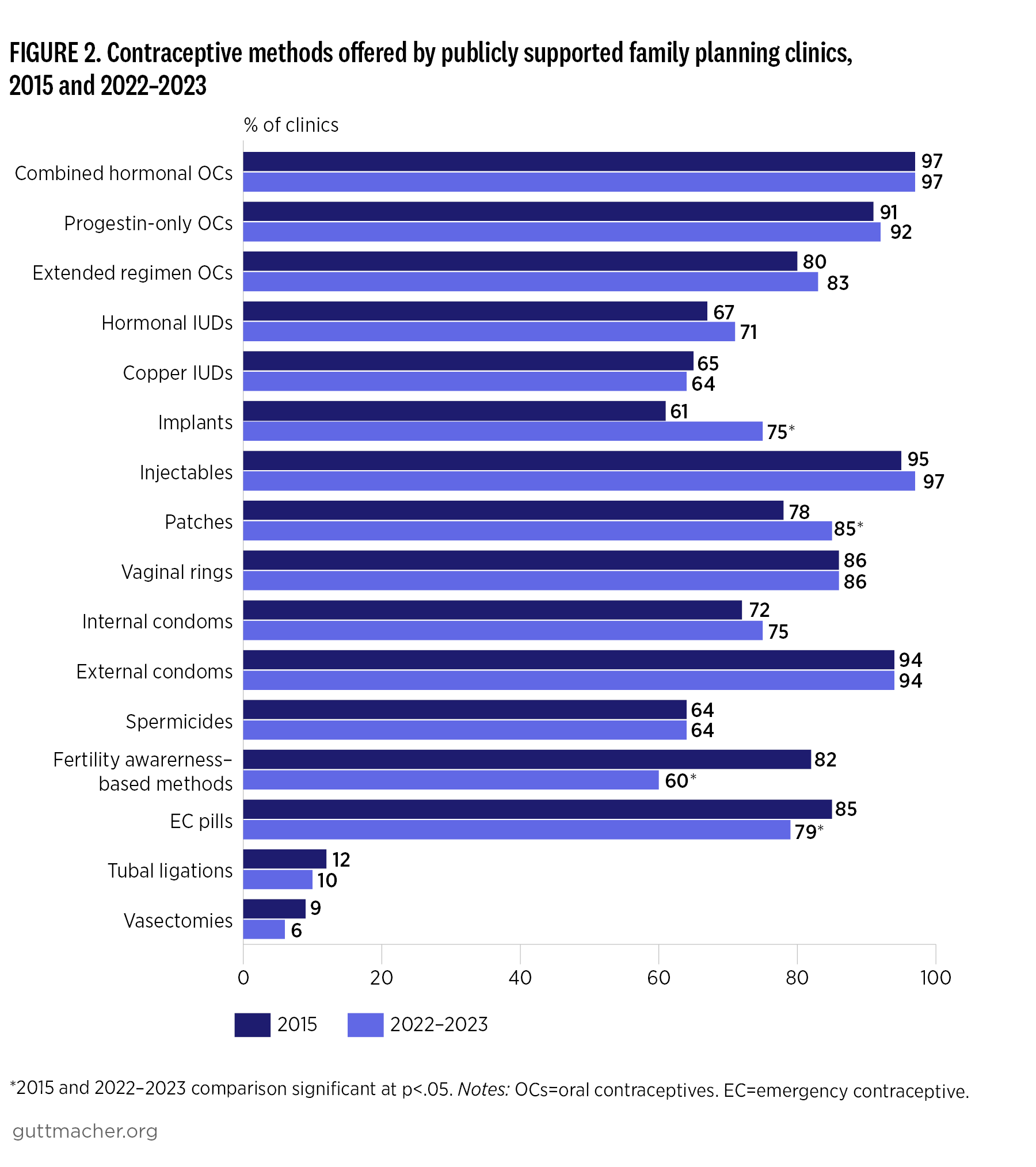
In 2022–2023, publicly funded family planning clinics provided a broad range of reversible contraceptive methods, including the 14 specific methods listed in the survey: combined hormonal oral contraceptives, progestin-only oral contraceptives, extended regimen of combined or progestin-only oral contraceptives, hormonal IUDs, copper IUDs, implants, injectables, patches, vaginal rings, internal condoms, external condoms, spermicides, fertility awareness–based methods (FABMs) and emergency contraceptive pills.
Overall, each reversible contraceptive method is provided by at least 60% of facilities. Provision of most contraceptive methods stayed about the same between 2015 and 2022–2023.
- All of the Planned Parenthood clinics in our sample offered provision of seven of the 14 methods, and more than 90% of these sites offered six of the remaining seven reversible methods (Appendix Table 1).
- There were slight increases in provision for implants and patches among most clinic types and decreases for FABMs and emergency contraceptive pills, especially among health departments and FQHCs between 2015 and 2022–2023 (Figure 2).
- The increase in implant provision was seen among all clinic types; the largest increases came among health departments and hospital and other clinic types. The increase in the provision of patches was driven by Planned Parenthood clinics and hospital and other clinic types.
- The decrease in FABM provision was seen among health departments (92% to 73%), Planned Parenthood facilities (92% to 81%), and FQHCs (75% and 50%), and the decrease in emergency contraception was driven by FQHCs (80% to 68%).
- Seventy-eight percent of facilities reported providing any LARC methods, which was roughly the same as in 2015.
- At least three-quarters of each facility type reported providing any LARC methods (the lowest among FQHCs); virtually all Planned Parenthood clinics provided LARC methods.
Three-quarters of facilities reported providing 10 or more reversible contraceptive methods in 2022–2023, which was roughly the same as in 2015 (Appendix Table 2).
- Each clinic type reported that approximately two-thirds of their facilities provided 10 or more reversible methods, and virtually all Planned Parenthood facilities provided 10 or more methods.
The proportion of clinics offering the full range of reversible methods remained steady between 2015 and 2022–2023. Overall, 62% of all clinics offered the full range of methods on-site in 2022–2023. A large majority, 80%, of reproductive health–focused clinics met the Healthy People 2030 objective of offering the full range of reversible contraceptive methods, compared with only 50% of primary care–focused sites; this was roughly the same as in 2015.
- As in 2015, a higher proportion of Planned Parenthood clinics had met the Healthy People 2030 objective, compared with the proportion of other clinic types. However, hospital and other clinic types saw an increase in the proportion providing this range of methods, from 59% in 2015 to 77% in 2022–2023.
Practices to increase contraceptive access and use
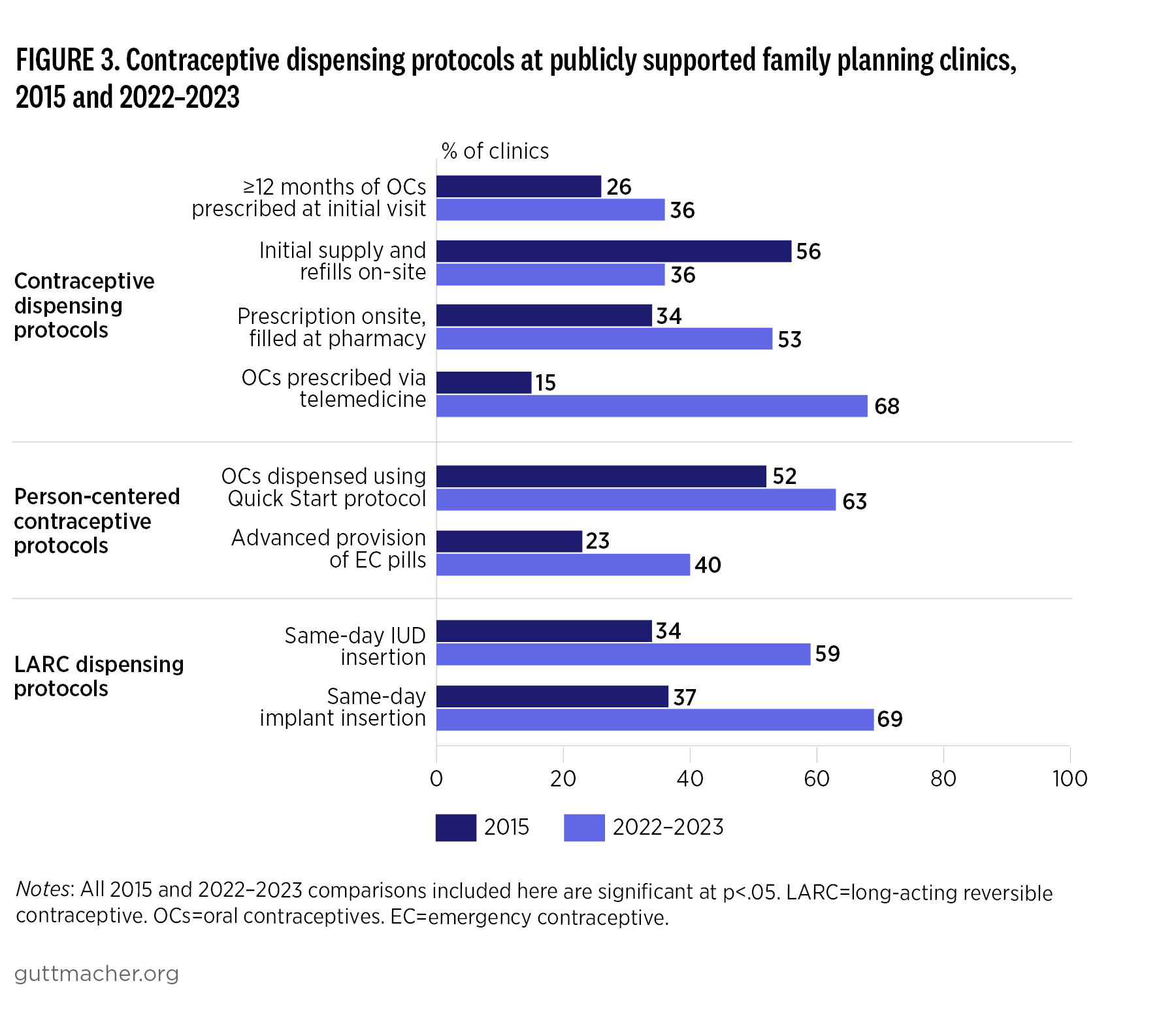
Overall, slightly more than one-third of clinics reported prescribing an oral contraceptive supply of 12 months or more at an initial visit, compared with a supply of less than 12 months (Appendix Table 3 and Figure 3). This increased from 26% in 2015 and varied by provider type.
- Nearly all Planned Parenthood facilities (92%) prescribed a supply of contraceptive pills of 12 months or more in 2022–2023; this increased from 64% in 2015.
- The most dramatic shift was seen among health departments, where prescribing a supply of pills for 12 months or more at an initial visit increased from just 14% to almost half of clinics. Conversely, less than half of FQHCs and hospital and other clinic types reported a supply of 12 months or more, a proportion that remained steady since 2015.
The proportion of clinics dispensing oral contraceptives (both the initial supply and refills) on-site decreased dramatically, from 56%‡ in 2015 to 36% in 2022–2023.
- FQHCs were least likely to supply both the initial supply and refills of oral contraceptives on-site (14%). The greatest shift can be seen in Planned Parenthood clinics. In 2015, these facilities were the provider type most likely to provide both supplies of contraceptive pills on-site, doing so at 83%‡ of their locations; however, in 2022–2023 this dropped to 53%.
- A small proportion (11%) of clinics reported only dispensing the initial supply of pills on-site; refills had to be filled at an outside pharmacy. No changes were seen in the proportion of sites utilizing this protocol since 2015, or across clinic type or service focus.
Almost two-thirds of clinics reported using Quick Start, a same-day protocol, always or often in 2022–2023, an increase from around half in 2015.
- Hospital and other clinic types saw the greatest increase in usage of the protocol (from 49% to 76%). Almost all Planned Parenthood sites used this protocol always or often in 2022–2023; as in 2015, FQHCs remained the least likely to do so.
In comparing data from 2015 with data from 2022–2023, the proportion of clinics that reported the dispensing of oral contraceptives without requiring that a pelvic exam be performed remained roughly the same (58% vs. 62%).
- However, increases were seen at Planned Parenthood facilities and hospital and other clinic types (the two most likely clinic types to carry out this protocol).
- The proportion of clinics always or often dispensing or prescribing emergency contraceptive pills ahead of time for a patient to keep at home increased between 2015 and 2022–2023, overall and among all clinic types. Planned Parenthood facilities were most likely to carry out this advanced provision of emergency contraception (81%), while FQHCs were the least likely (28%).
In 2022–2023, 59% of clinics reported performing IUD insertions on the same day that method was requested, compared with approximately one-third in 2015.
- Health departments reported the greatest shift in this protocol, from 29% in 2015 to 72% in 2022–2023. Planned Parenthood remained the most likely clinic type to perform same-day IUD insertions, as almost all sites provided this service in 2022–2023.
The proportion of clinics performing the insertion of implants on the same day the method was requested also increased (from 37% to 69%).
- As was the case for same-day IUD insertions, almost all Planned Parenthood facilities reported utilizing this protocol, and health departments saw the greatest shift between 2015 and 2022–2023 (from 30% to 76%).
Overall, there was an increase in the proportion of clinics offering prescriptions for oral contraceptives via telemedicine, from 15% in 2015 to 68% in 2022–2023.
- Increases were seen among all clinic types. The most notable increase came among Planned Parenthood clinics, which reported that 83% of their sites offer this service, compared with just 9% in 2015.
Trends in service provision
Publicly funded clinics that offer contraceptive care also offer a range of sexual and reproductive health and other general health care services. In both the 2015 and 2022–2023 surveys, clinic staff were asked about the availability of a wide range of health and social services at their facilities.
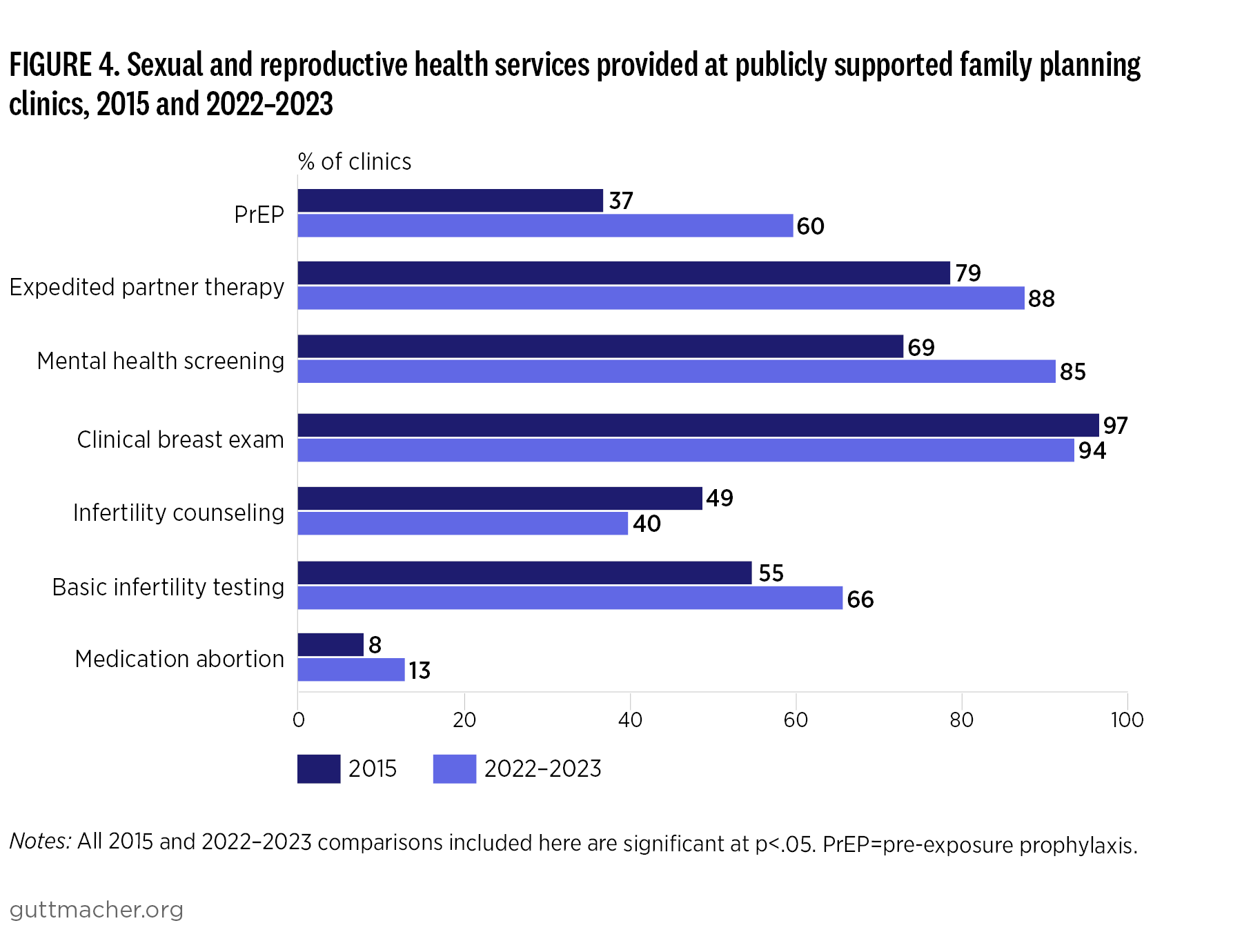
In this section, we present the results only for those services that were part of both surveys. There was no overall marked change between 2015 and 2022–2023 in the availability of primary care, STI/HIV testing and treatment, Pap smears, HPV vaccinations, colposcopy, mammography, pregnancy services or procedural abortions§ (Appendix Table 4). In 2022–2023, availability of certain sexual and reproductive health services varied by clinic type (Figure 4).
Primary care
Primary care was reported as available at nearly two-thirds of publicly funded family planning clinics in 2022–2023; there was no change from 2015. Primary care was far more likely to be offered at FQHCs (96%) than at any other clinic type, and health departments were least likely to offer this service (17%).
STI/HIV services
An overwhelming majority of clinics in our sample (94–98%) reported providing STI testing, including testing for HIV, chlamydia, gonorrhea and syphilis, and STI treatment in 2022–2023, which was roughly the same as in 2015. Availability of PrEP for HIV prevention increased across survey years, from a little more than one-third in 2015 to 60% in 2022–2023. This increase was seen across all clinic types; Planned Parenthood clinics reported the largest change, from 25% to 97%. Conversely, only one-third of health departments reported offering PrEP in 2022–2023.
Expedited partner therapy for STIs also increased between 2015 to 2022–2023; increases were seen among health departments (73% to 86%), and hospital and other clinic types (79% to 95%).
HPV vaccination
In 2022–2023, 92% of clinics reported offering HPV vaccinations, and there were some differences across clinic type: Every Planned Parenthood clinic (100%) offered HPV vaccinations, while slightly less than three-fourths (73%) of hospital and other clinic types offered this service.
Mental health screening
Mental health screening was offered at 85% of clinics in 2022–2023, an increase from more than two-thirds in 2015. Mental health screenings were reported to be available at almost all FQHCs (98%), but less than two-thirds (59%) of health departments. Planned Parenthood clinics saw the largest increase, from offering mental health screening at 29% of clinics in 2015 to 82% in 2022–2023.
Cervical cancer screening
Almost all clinics reported availability of Pap smears in 2022–2023 and 2015. A little more than one-third of clinics in 2022–2023 reported availability of colposcopies; there was no change from 2015. Colposcopies were least likely to be offered at health departments (12%), as compared with more than half of Planned Parenthood clinics.
Breast cancer screening
Overall availability of clinical breast exams decreased slightly, from 97% in 2015 to 94% in 2022–2023. This change was most noticeable for health departments, which were least likely to offer breast exams in 2022–2023: Availability of breast exams dropped from 97% to 86%. In 2022–2023, 100% of Planned Parenthood clinics reported offering clinical breast exams.
However, fewer than one in four clinics reported offering mammography in 2022–2023. FQHCs were most likely to provide this service (27%), compared with only 4% of Planned Parenthood clinics.
Infertility services
While two-thirds of clinics offered basic infertility testing in 2022–2023, an increase from 55% in 2015, the proportion of clinics offering infertility counseling dropped from about half (49%) in 2015 to 40% in 2022–2023. FQHCs were most likely to offer basic infertility testing in 2022–2023; almost three-fourths of this type of clinic reported the service to be available.
However, FQHCs were the least likely to offer infertility counseling; only one-third of FQHCs reported counseling availability, compared with 63% of Planned Parenthood clinics.
Pregnancy services
Almost all clinics offered pregnancy testing in 2022–2023, which was roughly the same as in 2015. More than eight in 10 clinics also reported availability of preconception counseling in 2022–2023. Provision of preconception counseling decreased among health departments, from 94% to 86%, while the availability of this service increased among hospital and other clinic types (from 86% to 95%).
Lower proportions of clinics in 2022–2023 offered prenatal care (44%) or breastfeeding counseling and support (61%), although this varied substantially by clinic type.
- While almost 60% of FQHCs reported availability of prenatal care, Planned Parenthood clinics were much less likely to offer this care (3%). Similarly, approximately two-thirds of FQHCs and health departments offered breastfeeding counseling and support, while only 9% of Planned Parenthood clinics provided this service.
Abortion services
Overall availability of medication abortion at publicly funding family planning clinics has remained low but increased from 8% in 2015 to 13% in 2022–2023 (Appendix Table 4).
- This change was most substantial for hospital and other clinic types, where availability increased from 8% in 2015 to 23% in 2022–2023. The highest proportion of medication abortion provision was among Planned Parenthood facilities (57%); markedly lower percentages of the other clinic types provided this service.
Fewer clinics overall (4%) offered procedural abortion services; there was no change from 2015.
- Health departments and FQHCs did not report availability of procedural abortion, while one in four Planned Parenthood clinics reported offering the service in 2022–2023.
Variation by Clinic Service Focus
Reproductive health–focused facilities served more patients for contraceptive services. Almost three-quarters of reproductive health facilities reported that more than 50% of their patients receive contraceptive services compared with 11% of primary care and other facilities (Appendix Table 1). However, compared with reproductive health facilities, more primary care and other facilities (46% vs. 27%) reported offering extended office hours. Primary care and other facilities were open an average of 10 more hours a week than their reproductive health counterparts.
A higher proportion of reproductive health–focused clinics provided oral contraceptives (combined hormonal and progestin-only), IUDs, implants, injectables, rings, condoms, FABMs and emergency contraceptive pills, compared with the proportions of primary care and other clinics (Appendix Table 2).
More reproductive health clinics reported providing patients with 12 months or more of contraceptive pills at their initial visit (51%), compared with primary care clinics (27%), and were more likely to provide the initial supply for pills and refills on-site (Appendix Table 3). Reproductive health–focused clinics provided higher proportions of most person-centered-care dispensing protocols and same-day LARC insertion than primary care clinics.
In terms of health services, reproductive health clinics were less likely to provide primary care, PrEP, HPV vaccination, mental health screening, mammography, prenatal care, and breastfeeding counseling and support than primary care and other facilities (Appendix Table 4). However, a higher proportion of reproductive health clinics provided STI treatment and expedited partner therapy, infertility counseling, pregnancy testing, preconception counseling and abortion.
Discussion
Publicly funded family planning clinics continue to fill a crucial role in the health care system, offering affordable contraceptive care and other sexual and reproductive health services. However, there are differences in service provision and contraceptive dispensing protocols among clinic types, as well as some evidence of increased strain on these safety-net clinics.
Overall, while clinic characteristics have largely remained stable from 2015 to 2022–2023, the availability of same-day appointments has declined by half. In addition, the average number of days new patients wait for an initial contraceptive service visit has doubled since 2015. This trend is driven by increases among FQHCs and Planned Parenthood facilities, the latter of which saw an increase in wait times from one to six days. These shifts occurred as the Title X program continues to be underfunded.5,13 While the ACA helped increase the number of people insured in the United States, an estimated 26 million individuals remain uninsured.14 For those without insurance, the underfunding of Title X leads to reduced access to high-quality sexual and reproductive health care.
Access to SRH care also decreased as a result of the gag rule implemented by the Trump administration, which continues to affect sexual and reproductive health care, even though the Biden administration rescinded the restrictions. The decline in availability of same-day appointments occurred across all clinic types, but was particularly large among Planned Parenthood clinics. In addition to the disruption caused by the gag rule, the decline in same-day appointments may reflect the strain on Planned Parenthood affiliates as they grapple with the wave of abortion restrictions imposed following the Supreme Court’s Dobbs decision and adjust service offerings and staffing across sites accordingly.
The availability of contraceptive methods over time has remained largely stable; there are no changes in the proportions of clinics offering at least 10 reversible methods or any LARC method. The only methods with increased availability over time were implants, which were more widely available among all clinic types in 2022–2023 than in 2015, and patches, whose use increased at Planned Parenthood facilities and hospital and other clinics.
Conversely, availability of FABM instruction or supplies decreased among all clinic types. This change could stem from shifting demand for fertility awareness–based methods, although it may also reflect changes to the item wording in our survey, as the 2015 survey asked about “natural family planning” rather than FABMs. In addition, availability of emergency contraception at publicly funded family planning clinics declined since 2015, driven by reduced availability at FQHCs, although certain forms of emergency contraception are available over the counter. Both of these declines represent decreased availability of person-centered care for patients, as availability of all methods is one crucial component of person-centered contraceptive care.15
Recognizing the importance of contraceptive choice, the US Department of Health and Human Services has identified as one of its Healthy People 2030 developmental objectives the on-site provision by publicly funded family planning clinics of the full range of reversible contraceptive methods (including oral contraceptives, IUDs, implants, injectables, patches, vaginal rings, external condoms, internal condoms, spermicide, other barrier methods and emergency contraceptive pills).16 Only hospital and other clinics have made gains in the proportion of sites that meet the Healthy People objective since 2015; although a higher proportion of Planned Parenthood facilities continue to meet the objective compared with other clinic types (94% of Planned Parenthood clinics vs. 77% of hospital and other clinics, 65% of health departments and 52% of FQHCs).
The use of several contraceptive dispensing protocols that support patient access has increased overall, including prescribing at least 12 months of oral contraceptive pills at the initial visit, offering both pills and refills on-site, dispensing oral contraceptive pills using the Quick Start protocol and advanced provision of emergency contraception. There remains wide variation in method availability and use of dispensing protocols that support patient access to contraceptives across clinic types.
Planned Parenthood facilities continue to exhibit the widest selection of contraceptive methods. Of these clinics, 99% offer at least 10 reversible methods, compared with 84% of hospital and other clinics, 80% of health departments and 64% of FQHCs. Similarly, more than 90% of Planned Parenthood clinics report following patient-centered dispensing protocols, including prescribing 12 months or more of contraceptive pills, dispensing these pills using the QuickStart protocol, dispensing them without a pelvic exam, providing emergency contraception in advance, and offering same-day insertion of both implants and IUDs. While other clinic types have increased their use of patient-centered contraceptive practices over time, health departments and FQHCs continue to lag other clinic types in using these dispensing protocols.
In addition, the use of telemedicine to dispense oral contraceptive pills rose dramatically from 2015 to 2022–2023, likely driven by the increased use of telemedicine during the COVID-19 pandemic. Only 15% of clinics reported using telemedicine to prescribe contraceptive pills in 2015, whereas more than two-thirds reported doing so in 2022–2023, indicating that the use of telemedicine has continued beyond the height of the pandemic.
The rapid uptake of telemedicine led to some challenges, but its use also reduces some barriers to care. Some patients may prefer telemedicine appointments, but some evidence suggests that perceived quality of care may be lower than for in-person appointments, so continued efforts to improve telemedicine use for contraceptive access are needed.8,17,18
The availability of general health and other sexual and reproductive health services has also remained largely stable, although availability of PrEP and mental health screening increased notably since 2015. The increase in PrEP availability was driven largely by Planned Parenthood facilities; a quarter of sites offered PrEP in 2015, while nearly all did so in 2022–2023. Other clinic types, particularly health departments, continue to have more limited availability,
Mental health screenings also increased among clinics overall, driven by increases among Planned Parenthood facilities, and, to a lesser extent, among health departments. These increases may reflect a growing acknowledgment of the important links between reproductive health and mental health.19 Medication abortion has also become more widely available at family planning clinics since 2015, driven largely by increased availability among hospital and other clinics, where availability nearly tripled from 8% to 23%, and it has remained available at more than half of Planned Parenthood clinics.
Limitations
While this report highlights important trends in the delivery of services among publicly supported family planning clinics in the United States, there are some limitations to our data. Most notably, the response rate for our survey was 24%, a marked decrease from the 2015 response rate of 50%.
Our response rate was particularly low among FQHCs. The decline in response rates was not due to decreased effort in fielding the survey; rather, we surmise that upheaval in the family planning clinic network, particularly among Title X–funded clinics resulting from the domestic gag rule, led to increased family planning clinic staff turnover and increased strain on clinic services, which in turn made it more difficult to reach the appropriate staff at clinic sites to complete the survey.
In addition, although we initially stratified our sample by Title X status, intending to weight our analyses accordingly and compare clinics by Title X status, we found too many discrepancies between the reported Title X status on our survey and in Guttmacher’s Family Planning Database.
These discrepancies likely stem from the disruption to the Title X program following the Trump administration’s gag rule, which resulted in more than one-quarter of Title X–funded sites (as of 2018) exiting the program by 2020. While some of these clinics have rejoined Title X since the Biden administration passed a new Title X Final Rule in 2021, these disruptions led to uncertainty and ongoing flux among sites that were in and out of the program in short periods of time.
It proved impossible to use Title X status as a weight variable, given ongoing changes to both the denominator (the universe of publicly funded family planning clinics) and the numerator in terms of Title X statuses in our sample. Also, our survey instrument was lengthy, and some respondents may have chosen to skip certain questions as a result. Finally, although our unit of analysis is the clinic, most surveys are completed by one staff member, and respondents likely vary with respect to their knowledge of the survey items, leading to variation in the accuracy of survey responses.
Despite these limitations, our survey reports on crucial trends in service delivery based on a nationally representative sample of clinics.
Conclusion
Publicly funded family planning clinics continue to provide essential sexual and reproductive health care, despite recent obstacles such as the domestic gag rule, COVID-19 and the Dobbs decision. Contraceptive method availability has remained largely stable since 2015, and Planned Parenthood clinics continue to have the widest availability of contraceptive methods compared with other clinic types. Wait times for appointments have increased substantially and the availability of same-day contraceptive appointments has declined by half. Supporting these safety-net clinics is crucial for ensuring equitable access to contraceptive and other sexual and reproductive health care.
Methodology Appendix
Sample
Between November 2022 and December 2023, we surveyed a nationally representative sample of 2,146 clinics providing publicly supported contraceptive services. The sample was drawn from the Guttmacher Institute’s family planning clinic database, which includes all known sites in the United States (N=10,454 sites at time the sample was pulled). The database is regularly updated using directories from Title X–supported clinics, Planned Parenthood affiliates and federally qualified heath centers (FQHCs), as well as personal communications with grantee and agency administrators.
Clinics were randomly selected within the eight possible categories (four clinic types and two Title X status possibilities). Due to differences in the overall number of clinic types and Title X status combinations, we varied the proportion sampled by category based on the total number in the category and the response rate for that category in the 2015 survey. We randomly sampled 48% of Planned Parenthood facilities, 28% of hospital and other clinics, 20% of health departments and 16% of FQHCs. Our sample was stratified by Title X status (received Title X funding or not) and clinic type (FQHCs, Planned Parenthood clinics, health departments and hospital and other clinics). As a result of missing data, Ns for survey items vary.
Data collection protocols
We programmed and hosted the online survey using Qualtrics; the survey took about 20–30 minutes to complete. Respondents did not have to answer specific questions or could stop taking the survey at any time. Participation in the study was voluntary, and respondents received a $50 gift card for their participation (remuneration was raised to $100 in the last two months of fielding). Our study procedures were reviewed by the chair of the Guttmacher Institute’s Institutional Review Board (IRB) and were deemed exempt from IRB review, as the data were collected from respondents in their professional capacity and do not include patient-level data.
For this study, respondents were eligible if they were family planning directors or administrators at publicly supported clinics providing family planning services in 2022–2023. Our fielding team reached out to each randomly sampled clinic by phone and email five times on average; a link to the survey was sent by email, and, in a minority of cases, by physical mail or fax.
Key measures
Clinic characteristics
We asked clinics what type of organization the clinic is affiliated with (health department, Planned Parenthood, FQHC, hospital or other) and the main type of service provided by the clinic (reproductive health services, primary care or other). In terms of basic contraceptive provision, we asked approximately how many patients receive any contraceptive services at the clinic during a typical week (<5, 5–19, 20–49, 50–99, 100–199, ≥200); approximately what percentage of patients receive contraceptive services annually (2022–2023: <10%, 10–49%, ≥50%; 2015: <10%, 10–24%, 25–49%, 50–74%, 75–99%, 100%); the total number of hours the clinic is open for contraceptive service provision during a typical week; the number of days patients typically have to wait to get an initial contraceptive service appointment (same day, 1–7 days, more than seven days; in 2015, we asked whether it was same-day service, and if not, how many days or weeks); and if the clinic offers contraceptive services on Saturdays and/or Sundays and after 6 p.m. on any weekday (in 2015, we asked the number of hours clinics were open during these times).
Clinic finances
We asked if the clinic received Title X funding in the past five years (since January 2018), and for those who selected “yes,” we asked during which years the clinic received funding (in 2015, we only asked if the clinic received Title X funds at the time of the survey). We asked clinics for the distribution of patients paying for care using private insurance, public insurance or without insurance. In addition, we asked in the 2022–2023 survey if the clinic’s annual revenue had significantly declined since 2018 because of any of the following reasons: a cut in federal funding, a cut in state or local funding, a decrease in revenue from patient fees, a decrease in revenue from Medicaid reimbursements, a decrease in revenue from private insurance reimbursements or patient declines due to the COVID-19 pandemic.
Contraceptive methods
We asked, for each listed contraceptive method, whether the method is provided or prescribed at the site, patients are referred to another clinic or the method is not provided or referred for. The methods are the following: combined hormonal oral contraceptives, progestin-only oral contraceptives, extended regimen of either combined or progestin-only oral contraceptives (e.g., Seasonale, Seasonique), hormonal IUDs (e.g., Mirena, Skyla), copper IUDs (e.g., ParaGard), implants (e.g., Nexplanon), injectables (e.g., Depo-Provera), patches (e.g., Ortho Evra), vaginal rings (e.g., NuvaRing), external (male) condoms, other barrier methods (e.g., diaphragm, cervical cap, sponge, internal condoms), spermicides, emergency contraceptive pills (e.g., Plan B, ella), tubal ligations (in 2015, we asked about female sterilization, including tubal ligations and Essure), vasectomies, and fertility awareness–based method instruction or supplies (FABMs) (e.g., cycle beads). In 2015, instead of asking about FABMs, we asked about natural family planning instruction or supplies.
Sexual and reproductive health services
We asked, for each listed health service, whether the service is provided or prescribed at the site, clients are referred to another clinic or the service is not provided or referred for. Listed health services asked on both surveys are the following: primary (general health) care, HIV testing, pre-exposure prophylaxis for HIV prevention, chlamydia/gonorrhea testing, syphilis testing, STI treatment, expedited partner therapy for STIs, Pap smear (conventional and/or liquid-based), HPV vaccination, mental health screening, colposcopy, mammography, clinical breast exam, breastfeeding counseling and support, infertility counseling, basic infertility testing (e.g., pelvic exam, hormone levels), pregnancy testing, prenatal care, preconception counseling, medication abortion and surgical abortion. While the survey asked about surgical abortion, we refer to this as procedural abortion in the report.
Dispensing protocols
We asked clinics that reported prescribing hormonal oral contraceptives how many total months (i.e., cycles) of these contraceptive pills are typically provided and/or prescribed at an initial contraceptive visit (1 month, 2–3 months, 4–6 months, 7–11 months or ≥12 months); in 2015, respondents were asked about the number of cycles instead of number of months. In terms of method for dispensing these pills, we asked whether most patients receive both the initial supply and additional refills at the clinic, most patients receive an initial supply at the clinic and a prescription to fill additional cycles at a pharmacy, most patients receive a prescription that they fill at a pharmacy or another dispensing/prescription method is used.
Pertaining to IUDs and implants, we asked in 2022–2023 if the insertion and removal of each respective method occurred in one visit (same day), two visits, or three or more visits; the 2015 survey asked whether IUDs, implants or injectables were injected or inserted during the same appointment in which the method was requested or during a follow-up appointment after the method was requested. We asked clinics how often (always, often, sometimes, rarely or never) the following dispensing protocols are employed for each method provided at their facility: oral contraceptives are dispensed using the Quick Start protocol (in which the patient takes first pill on the day of the visit, regardless of where they are in their menstrual cycle); new patients get oral contraceptives without having to get a pelvic exam; or emergency contraceptive pills are dispensed or prescribed ahead of time for a patient to keep at home (in 2015, we only asked sometimes, rarely or never). In terms of telemedicine and telehealth provision, we asked if clinics offer initial prescriptions for oral contraceptives via telemedicine; the 2015 survey asked whether these pills are prescribed over the phone (or Internet) without a clinic visit via telemedicine.
Response and weights
Among the sample of 2,146 clinics, we determined that 257 clinics had closed or stopped providing contraceptive services and were thus ineligible for the survey. In addition, 122 sites refused to participate, and we never received responses from 1,321 sites despite multiple attempts to contact staff. A total of 446 clinics completed the survey, corresponding to an overall response rate of 24%. The response rate varied by clinic type and Title X status, respectively: 53% for Planned Parenthood facilities, 34% for health departments, 20% for hospital and other clinics, 11% for FQHCs; and 46% for clinics receiving Title X and 11% for non-Title X clinics.
All cases were weighted for sampling ratios and nonresponse to reflect the universe of publicly supported family planning providers at the time the sample was drawn, and the results presented are nationally representative.
However, due to both the low response rate and the ongoing changes to the Title X network before and during fieldwork, we were unable to estimate reliable weights for clinics by Title X status. The results are therefore presented as national totals and separately according to clinic type and service focus, but not separately by Title X status.
Statistical analyses
Analyses were performed using Stata 18. We present descriptive statistics to summarize the data. We tested for significance using chi-square tests, linear regression and logistic regression to compare the data for 2015 with the data for 2022–2023 and to compare clinic types in 2022–2023. All comparisons mentioned in the text are statistically significant at the p<.05 level unless otherwise indicated, although some significant comparisons are not mentioned in the report.
Suggested Citation
VandeVusse A et al., Publicly Supported Family Planning Clinics in 2022–2023: Trends in Service Delivery Practices and Protocols, New York: Guttmacher Institute, 2024, https://www.guttmacher.org/report/publicly-supported-family-planning-clinics-2022-2023.
Acknowledgments
The authors gratefully acknowledge the clinic staff who participated in this study. In addition, we thank the following current or former colleagues at the Guttmacher Institute for reviewing project materials and providing research assistance: Nakeisha Blades, Ava Braccia, Joerg Dreweke, Amy Friedrich-Karnik, Liza Fuentes, Jennifer Frost, Megan Kavanaugh, Kathryn Kost, Laura Lindberg, Lauren Mitchell, Bashiru Mohammed, Dawun Smith and Mia Zolna. This report was edited by Peter Ephross. The findings and conclusions in this article are those of the authors and do not necessarily reflect the views of Planned Parenthood Federation of America, Inc.
This study was made possible by grants to the Guttmacher Institute from two anonymous donors and by the Office of Population Affairs (OPA) of the US Department of Health and Human Services (HHS) as one component of a financial assistance award from OPA totaling $2.25 million. For the clinic survey component, about 10% was funded by OPA and 90% was funded by nongovernment sources. The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement, by OPA, HHS or the US government. The findings and conclusions in this report are those of the authors and do not necessarily reflect the positions and policies of the donors.
Footnotes
*Percentages do not add to 100 because of rounding.
†Transgender men, gender-nonconforming and nonbinary people also become pregnant and need and use contraceptive services, but some data sources restrict data collection to cisgender women, so we use “women” in this report.
‡As a result of a change in data processing, this proportion has changed slightly from the 2015 published estimate.
§Although the surveys asked respondents about "surgical abortion," Guttmacher prefers the term "procedural abortion," which better describes current abortion methods.
References
1. Frost JJ et al., Publicly Funded Contraceptive Services at US Clinics, 2015, New York: Guttmacher Institute, 2017, https://www.guttmacher.org/report/publicly-funded-contraceptive-services-us-clinics-2015.
2. Frost JJ et al., Publicly Supported Family Planning Services in the United States: Likely Need, Availability and Impact, 2016, New York: Guttmacher Institute, 2019, https://www.guttmacher.org/report/publicly-supported-FP-services-US-2016.
3. Frost JJ, Mueller J and Pleasure ZH, Trends and Differentials in Receipt of Sexual and Reproductive Health Services in the United States: Services Received and Sources of Care, 2006–2019, New York: Guttmacher Institute, 2021, https://www.guttmacher.org/report/sexual-reproductive-health-services-in-us-sources-care-2006-2019.
4. Zolna MR and Frost JJ, Publicly Funded Family Planning Clinics in 2015: Patterns and Trends in Service Delivery Practices and Protocols, New York: Guttmacher Institute, 2016, https://www.guttmacher.org/report/publicly-funded-family-planning-clinic-survey-2015.
5. Dawson R, What federal policymakers must do to restore and strengthen a Title X family planning program that serves all, Guttmacher Policy Review, 2021, 24, https://www.guttmacher.org/gpr/2021/03/what-federal-policymakers-must-do-restore-and-strengthen-title-x-family-planning-program.
6. Hasstedt K and Dawson R, Title X under attack—our comprehensive guide, Policy Analysis, Guttmacher Institute, 2021, https://www.guttmacher.org/article/2019/03/title-x-under-attack-our-comprehensive-guide.
7. Lindberg LD et al., The Continuing Impacts of the COVID-19 Pandemic in the United States: Findings from the 2021 Guttmacher Survey of Reproductive Health Experiences, New York: Guttmacher Institute, 2021, https://www.guttmacher.org/report/continuing-impacts-covid-19-pandemic-findings-2021-guttmacher-survey-reproductive-health.
8. VandeVusse A et al., Disruptions and opportunities in sexual and reproductive health care: How COVID-19 impacted service provision in three US states, Perspectives on Sexual and Reproductive Health (University of Ottawa), November 2022, https://doi.org/10.1363/psrh.12213.
9. Frederiksen B, Gomez I and Salganicoff A, Rebuilding Title X: New Regulations for the Federal Family Planning Program, KFF, 2021, https://www.kff.org/womens-health-policy/issue-brief/rebuilding-title-x-new-regulations-for-the-federal-family-planning-program/.
10. Frederiksen B, Gomez I and Salganicoff A, Rebuilding the Title X Network Under the Biden Administration, KFF, 2023, https://www.kff.org/womens-health-policy/issue-brief/rebuilding-the-title-x-network-under-the-biden-administration/.
11. Friedrich-Karnik A and Easter R, Restricting Title X results in cascading harms, Policy Analysis, Guttmacher Institute, 2024, https://www.guttmacher.org/2024/08/restricting-title-x-results-cascading-harms.
12. Fowler C, Gable J and Lasater B, Family Planning Annual Report: 2021 National Summary, Washington, DC: Office of Population Affairs, Office of the Assistant Secretary for Health, Department of Health and Human Services, 2021, https://opa.hhs.gov/sites/default/files/2022-09/2021-fpar-national-final-508.pdf
13. Easter R, Friedrich-Karnik A and Kavanaugh ML, Any Restrictions on Reproductive Health Care Harm Reproductive Autonomy: Evidence from Four States, Guttmacher Institute, 2024, https://www.guttmacher.org/report/any-restrictions-reproductive-health-care-harm-reproductive-autonomy-evidence-four-states.
14. Sharer B and Lukens G, Health Coverage Rates Vary Widely Across—and Within—Racial and Ethnic Groups, Center on Budget and Policy Priorities, 2024, https://www.cbpp.org/research/health/health-coverage-rates-vary-widely-across-and-within-racial-and-ethnic-groups.
15. Holt K et al., Beyond same-day long-acting reversible contraceptive access: a person-centered framework for advancing high-quality, equitable contraceptive care, American Journal of Obstetrics and Gynecology, 2020, 222(4):S878.e1-S878.e6, https://doi.org/10.1016/j.ajog.2019.11.1279.
16. US Department of Health and Human Services, Increase the Proportion of Publicly Funded Clinics That Offer the Full Range of Reversible Birth Control—FP‑D01, https://health.gov/healthypeople/objectives-and-data/browse-objectives/family-planning/increase-proportion-publicly-funded-clinics-offer-full-range-reversible-birth-control-fp-d01.
17. Kavanaugh ML and Zolna MR, Where Do Reproductive-Aged Women Want to Get Contraception?, Journal of Women’s Health, 2023, 32(6):657–669, https://doi.org/10.1089/jwh.2022.0406.
18. Lindberg L et al., Telehealth for contraceptive care during the COVID-19 pandemic: results of a 2021 national survey, American Journal of Public Health, 2022, 112(S5):S545-S554, https://doi.org/10.2105/AJPH.2022.306886.
19. Hall KS et al., Contraception and mental health: A commentary on the evidence and principles for practice, American Journal of Obstetrics and Gynecology, 2015, 212(6):740–746, https://doi.org/10.1016/j.ajog.2014.12.010.
Additional Downloads
- 2022-2023 Survey of Clinics Providing Contraceptive Services publicly-supported-family-planning-clinics-2022-2023-survey.pdf
- Appendix Tables publicly-supported-family-planning-clinics-2022-2023-appendix_tables-excel.xlsx