The number of STIs is increasing in the United States, especially among adolescents and young adults. In 2018, combined cases of syphilis, gonorrhea and chlamydia reached an all-time high after rising for the fifth year in a row.1 Between 2014 and 2018, cases of chlamydia, one of the most common STIs, increased by 15%.2 Although less prevalent overall, gonorrhea and syphilis increased by 35%3 and 50%,4 respectively.
Over the five years that this trend has emerged, socially conservative policymakers have remained intent on limiting young people’s access to sexual health information and services. These efforts stem from the disingenuous claim that such access will encourage adolescents to have more sex with more people, even though a robust body of research indicates otherwise.5,6 Social conservatives’ arguments stigmatize sex outside of marriage, shame sexually active young people (particularly young women), and intentionally ignore the fact that sex is a normal part of adolescence and adulthood.
Researchers have not established the full set of factors driving the rising prevalence of STIs among young people, but they have several theories, including decreased condom use; declining local, state and federal investment in STI programs; expanding sexual networks facilitated by dating apps; the rise of antibiotic-resistant strains of certain STIs; and, potentially, increased testing.7–11
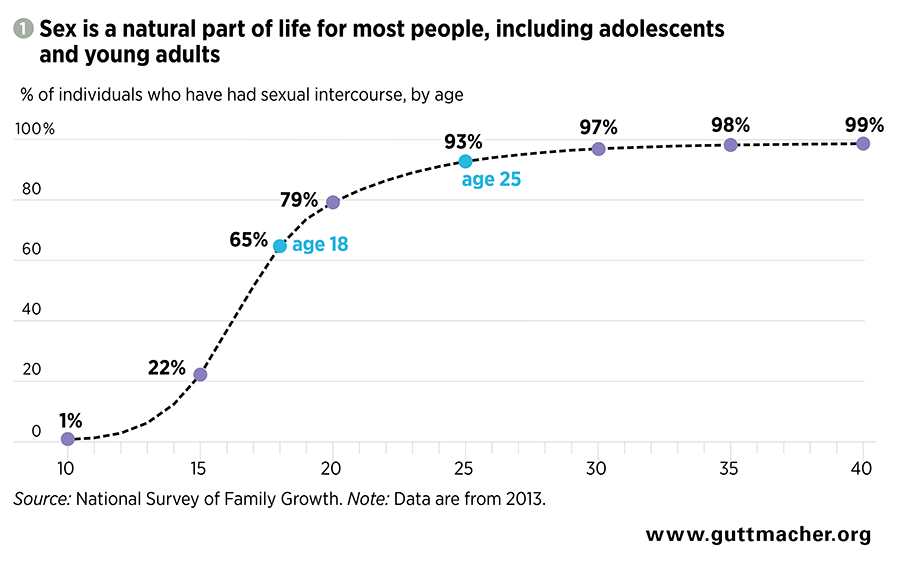
Sex is a part of many adolescents’ and young people’s lives: In the United States, two-thirds of 18-year-olds have had sex, and by age 25, more than nine in 10 people will have had sex (see figure 1).12 Preventing and treating STIs—including through education on healthy sex and relationships, routine screenings, disease management and prevention—must be a part of health care for young people.
Young People Are Vulnerable to STIs
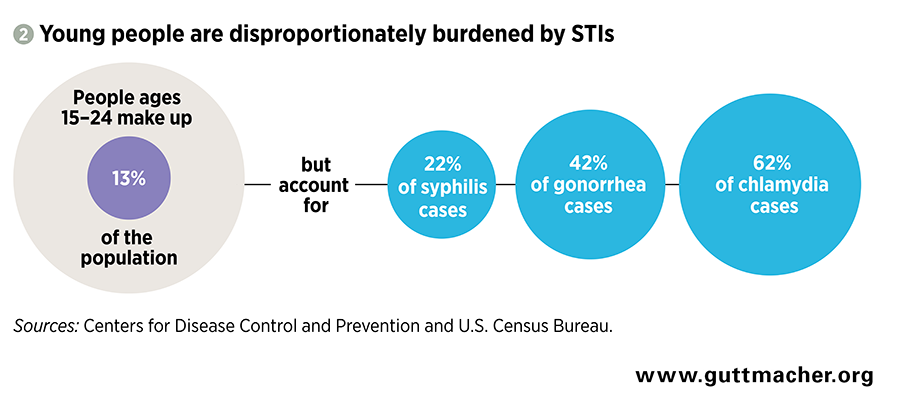
Adolescents and adults in their early 20s have been disproportionately impacted by the recent rise in STIs. Young people in this age-group acquire an estimated half of all new STIs annually, yet they make up only one-quarter of the sexually active population.13 In 2018, people aged 15–24 represented a substantial proportion of all those with chlamydia (62%),2 gonorrhea (43%)3 and syphilis (22%)4 (see figure 2).14 Although the Centers for Disease Control and Prevention (CDC) recognizes over a dozen STIs,15 these three are the major ones (besides HIV) that it tracks. When left untreated, these infections can cause infertility, poor pregnancy and birth outcomes, and increased risk of acquiring new or transmitting existing STIs, especially HIV.16
Some groups of young people in the United States face inordinately high rates of STIs. Young men who have sex with men are at higher risk of obtaining a new STI than the general population due to the structure of their sexual networks, decreased access to screening and treatment, and stigma.17 Black (and to a lesser degree, Hispanic and Native) adolescents and young adults are substantially more likely than their peers to be living with an STI.18 These disparities arise not from individual or population-level behavioral differences, but structural barriers such as racism, discrimination and poverty that can block people of color from accessing affordable and high-quality health care, including the sexual health services that are necessary to prevent and treat STIs.18,19 Some groups, like black men who have sex with men, have particularly high rates of STIs in part because they face multiple forms of discrimination.20
In general, people in their teens and early 20s are at risk of contracting STIs for a combination of biological, logistical and behavioral reasons. Adolescent girls and young women are particularly susceptible to infection for some STIs, such as chlamydia, because of the cellular makeup of their cervixes.21 Adolescents and young people who are insured as dependents on their parents’ health plans may be reluctant to disclose their sexual behavior to health care professionals because of confidentiality concerns, which may decrease the likelihood that they receive STI screening and treatment and increase their risk of passing STIs to others. Lack of transportation, insurance coverage and funds to pay for services may also keep young people from accessing the STI care that they need. Finally, many adolescents and young adults have multiple sexual partners, which increases their risk of exposure to STIs.22
Key Interventions and Barriers to Receiving Care
Interventions to support high-quality information and care related to STIs include sex education programs, testing and treatment services, preventive technologies and vaccines, and supportive and dignified care. Unfortunately, young people face barriers in all of these areas.
Provide sexual health information. Young people deserve accurate and complete sex education in order to avoid STIs and mitigate their effects. Programs should provide students with accurate information about the prevention, transmission, symptoms and treatment of STIs. They should also equip students with skills to foster healthy relationships and express their sexual autonomy in a healthy way, such as by understanding consent and being able to advocate for condom use. The sexual health information provided should be age appropriate as well as responsive to and respectful of a range of cultural backgrounds, sexual orientations and gender identities.
One major barrier to accurate and complete sex education has been conservatives’ promotion of abstinence-only programs. These programs take an all-or-nothing approach to STI prevention that discourages condom use, is not in line with adolescents’ sexual activity and does not prepare them for sex in adulthood (see New Name, Same Harm: Rebranding of Federal Abstinence-Only Programs, 2018). Proponents of abstinence frame this approach as the only certain way to avoid STIs, but they fail to note that many adolescents who attempt to abstain from sex will ultimately have sex before marriage.6 In fact, longitudinal research shows that when adolescents who have attempted to abstain do have sex, many do not use condoms that would protect them from STIs.
Abstinence-only programs not only withhold important information from young people, but can actively harm them. This approach sends adolescents the message that sex outside of marriage is shameful or inherently dangerous, perpetuates gender stereotypes, ignores the experiences of LGBTQ youth and promotes a narrow view of an acceptable life course (i.e., marriage, then sex, then parenthood).23 Further, restricting sex education to a few topics contributes to misinformation and stigma that prevents adolescents and young people from seeking information and care related to STIs.
Congress, with the support of the Trump administration, has been gradually increasing funding for abstinence-only education, and funding reached a 10-year high of $110 million in 2019.24 Moreover, 29 states require that abstinence be stressed in sex education programs, and 19 states require instruction on the purported importance of engaging in sexual activity only within marriage.25
Ensure testing and treatment. It is critical that adolescents and young people receive accessible and high-quality STI testing and treatment services. The majority of STIs are asymptomatic or have nearly undetectable symptoms, so routine screening is necessary to prevent the development of disease and transmission to additional people.26
Adolescents and young adults face particular barriers in accessing testing and treatment services. Young people in schools or workplaces with inflexible schedules will have difficulty visiting clinics that keep regular business hours, while those without a car or another convenient, safe and affordable source of transportation may be entirely cut off from care. Adolescents who make it to a clinic face another, emerging challenge: untreatable STIs. Antibiotic-resistant strains of gonorrhea are particularly common, although drug resistance has been found in other STIs as well.27
STI clinic funding has been hampered in recent years by federal, state and local policies. The CDC’s STI prevention and treatment budget has been flat since 2003, resulting in a 40% decrease in funds when adjusted for inflation.9 And in 2012, budget cuts affecting half of all state and local STI programs forced almost two dozen local health departments around the country to close their STI clinics, while more than 50% of the remaining state and local health departments experienced budget cuts, leading to reduced clinic hours, screening services or tracing efforts to find people who may have had infections.28 In 2019, one-quarter of all Title X family planning sites (representing nearly half of all patients served by the program nationally) left the program after the Trump administration transformed it from one that supported high-quality, low-cost sexual and reproductive health care to one that restricts providers’ ability to offer a full range of services.29 This is a huge loss for a program that, in 2018, served 1.6 million people younger than 25 and provided over one million chlamydia tests to that age-group.30
Offer preventive care. Public health practitioners approach STI prevention from two angles: preventing individuals from obtaining an infection in the first place, and preventing them from spreading it to others. Key methods of prevention include condoms, vaccines and expedited partner therapy, in which a provider supplies prescriptions or medications to a patient’s partners without first diagnosing the partners.
Condoms are the most effective and popular way for sexually active people to prevent STIs, but there is room for improvement. Between 2013 and 2017, condom use gradually declined among high schoolers.31 Experts hypothesize that increased reliance on other HIV-prevention methods (such as preexposure prophylaxis, or PrEP) and long-acting reversible contraceptive methods are driving this trend, but acknowledge that further research is needed. Reliance on condoms is limiting because they are currently the only method available to simultaneously prevent pregnancy and the spread of STIs. Not having a wider selection of multipurpose prevention technologies undermines STI prevention efforts and makes STI prevention difficult for people who do not or cannot use condoms.
The paucity of STI vaccines is another barrier to prevention. There are currently only vaccines for hepatitis A, hepatitis B and some strains of HPV.32 The HPV vaccine demonstrates the potential power of an STI vaccine: Since its introduction in 2006, HPV infections have declined among adolescent girls by 71% and women in their early 20s by 61%,33 despite the fact that uptake of the HPV vaccine has lagged behind other vaccines for adolescents.34,35
Guarantee dignified and supportive care. STI prevention, testing and treatment are highly stigmatized topics that young people are often reticent to discuss, but providers and insurers have an opportunity to create an environment in which all patients feel respected and cared for. Such a climate would allow young patients to meet with providers without their parents’ permission or knowledge. Further, providers and insurers should have the training and resources to recognize and respect patients with a variety of cultural backgrounds, sexual orientations and gender identities.
Unfortunately, conservative ideologies that stigmatize sexually active young people have been operationalized into policies that impact the quality of care available to them. The 2019 changes to the Title X national family planning program (known as the domestic "gag rule") intentionally stigmatize and alienate patients younger than 18 who have STIs, making it harder for them to get the care they need.36
Several types of state-level policies block adolescents from receiving confidential care or consenting to their own care. Laws in 18 states explicitly allow physicians to inform minors’ parents that they are seeking or receiving STI services and 12 states require minors to be of a certain age (usually 12 or 14) before being able to consent to non-HIV STI care on their own.37 These policies are harmful to adolescents as they are less likely to seek sexual or reproductive health care, including STI services, if they believe that their parents will find out about it.38
Confidentiality concerns related to health insurance may also dissuade adolescents and young adults from seeking care related to STIs. People insured as dependents, including adolescents and young people on their parents’ insurance plans, can have their confidentiality breached when an explanation of benefits form is automatically sent to the holder of the insurance policy (usually their parent) after a medical visit.39,40 The document provides a detailed description of services provided, meaning it can reveal that a dependent has been screened or treated for an STI.
Proactive Policy Recommendations
To address the rising tide of STIs among young people, policymakers and advocates should focus their efforts on a few key actions that will support high-quality sexual health information and care for all young people.
Prioritize care for marginalized youth. The Youth Access to Sexual Health Services Act would create federal grants to support the availability of high-quality sexual health services for vulnerable young people.41 The grants would serve people younger than 26 who are disadvantaged because of underlying structural barriers or social inequities. Given the higher prevalence of STIs among certain marginalized groups and the barriers to STI prevention and treatment that come along with marginalization, investing resources in programs that specifically serve these groups would have a high return.
Commit to high-quality sex education. The Real Education for Healthy Youth Act (REHYA) would redirect funds from the Title V abstinence-only grant program to a new grant program that funds comprehensive sex education programs in high schools, colleges and organizations that focus on adolescent health.42 Programs funded through this law would help young people make informed, responsible and healthy decisions throughout their lives, including by equipping them with skills to avoid STIs and communicate about STIs with their partners. Entities that serve groups disproportionately impacted by STIs would be given funding priority.
REHYA would zero out funding for the Title V abstinence-only program, but federal lawmakers should also zero out funding for the other federal abstinence-only education program ("Sexual Risk Avoidance Education"). State legislators have an opportunity to expand the scope of their sex education requirements to better meet the needs of young people. State lawmakers are increasingly pursuing legislation that emphasizes consent in sexual relationships, equips adolescents with skills to establish healthy relationships, and responds to the needs of young people with a range of sexual orientations and gender identities.43,44
Expand access to clinical care. Federal and state policymakers should invest resources in STI clinics in order to reduce the barriers to STI testing and treatment that many young people face. With additional funding, clinics could extend their hours, expand staff capacity and cover medical fees for patients who need financial assistance. Where feasible, clinics could also distribute at-home test kits that would allow patients to test for STIs on their own time and in a comfortable setting.45 Clinics could offer counseling and prescriptions remotely, meaning that the patient does not have to visit a clinic in person. On the federal level, the Title X gag rule should be rescinded and the program restored to its full capacity.29
Invest in preventive technology, vaccines and antibiotics. Adolescents and young adults would benefit from increased investment in research and development of technologies that offer protection against STIs. Internal and external condoms are currently the only mechanisms that allow people to simultaneously prevent pregnancy and STIs, but expanding young people’s options would enable them to find the method that best fits their wants and needs. A wider range of vaccines in general, along with efforts to improve uptake of the HPV vaccine, would also ensure broader protection against STIs. And as some STIs become resistant to current antibiotics, it is increasingly important to develop new and more effective treatment options.
Safeguard confidential care. Policies governing providers and insurance carriers should support young people’s confidentiality when seeking STI-related care. For example, every state should have policies stating that minors have the right to consent to STI care and receive that care without notice to their parents. If a provider uses electronic health records, that system should be designed within the confines of state and federal laws to protect adolescents and other patients insured as dependents (e.g., records are not automatically viewable by a parent, process for adolescent patients to affirmatively consent to sharing records with a parent). States should take steps to protect the confidentiality of people insured as dependents, such as by ensuring that explanation of benefits forms limit the detail provided for sensitive services such as STI care.40 Finally, adolescents and young adults must be informed of the level of confidential treatment they will receive before obtaining care.