Sex education is vital to adolescents’ healthy sexual development, and young people have the right to information that is medically accurate, inclusive, and age- and culturally appropriate in order to make informed decisions about their sexual behavior, relationships and reproductive choices.1–4 Numerous health organizations recommend comprehensive sex education that addresses a range of topics,2–4 and support for this type of instruction is reflected in national public health goals.5
Formal sex education for adolescents consists of instruction that generally takes place in a structured setting, such as a school, community center or church. The US Department of Health and Human Services’ Healthy People 2030 initiative includes objectives for formal sex education for adolescents based on a minimal set of topics that focus on delaying sex, using birth control methods and preventing STIs (including HIV).6 However, not all states require sex education and any required content varies widely; there is further variation at both the district and school levels.7,8 Understanding differences in the receipt of formal instruction is the first step toward ensuring that the needs of all youth are met.
The data in this fact sheet come from multiple rounds of the National Center for Health Statistics’ National Survey of Family Growth and apply to female and male respondents aged 15–19 at the time of the survey interview. (Self-reported gender at time of interview may differ from respondents’ gender assigned at birth.)
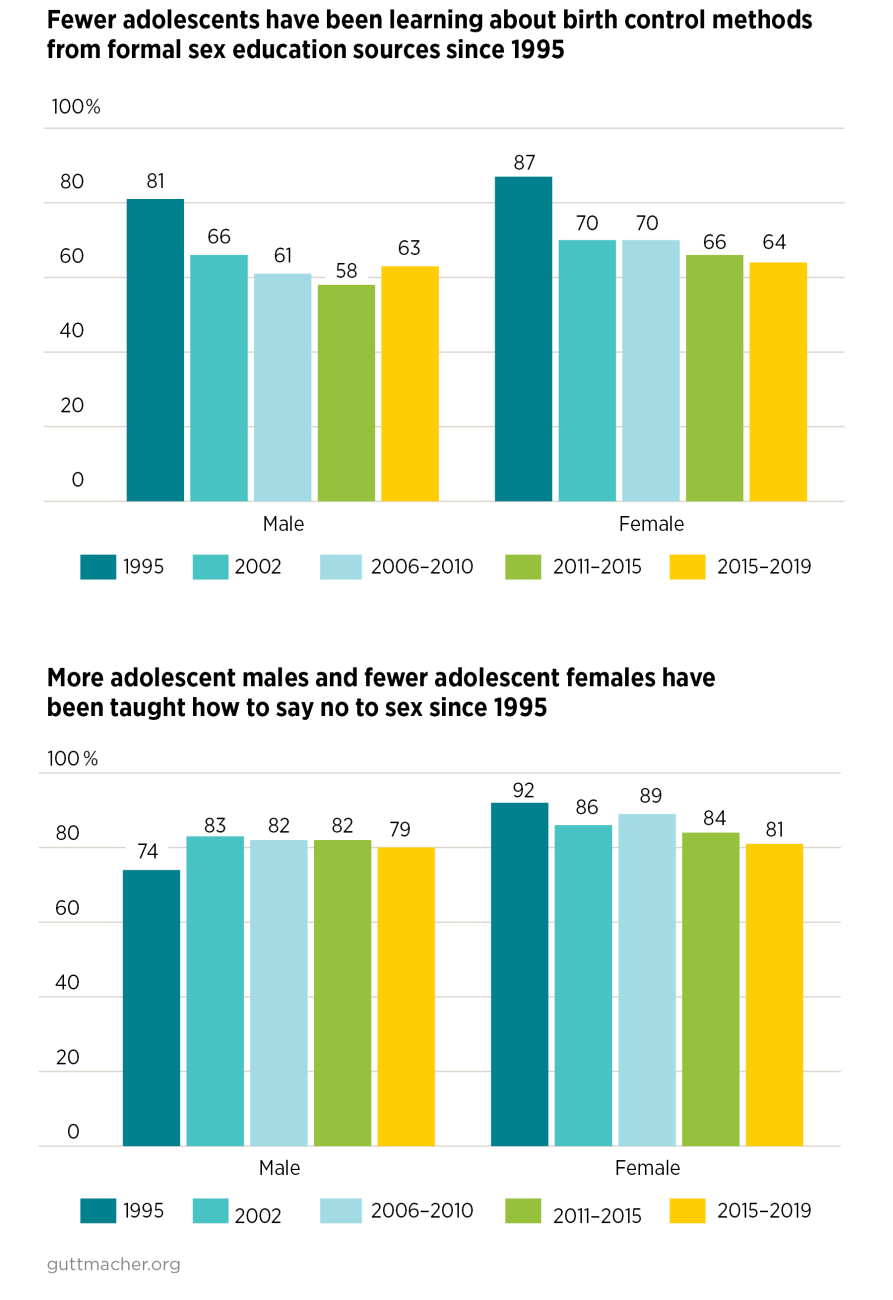
- Young people are not getting the sex education they need: About half of adolescents (53% of females and 54% of males) reported in 2015–2019 that they had received sex education that meets the minimum standard articulated in Healthy People 2030; among teens reporting penile-vaginal intercourse, fewer than half (43% of females and 47% of males) received this instruction before they first had sex.9
- In 2015–2019, more adolescents reported that they had received instruction about saying no to sex (81% of females and 79% of males) or waiting until marriage (67% and 58%, respectively) than about where to obtain birth control (48% of females and 45% of males) or how to use a condom (55% and 60%, respectively).9