Corrected July 16, 2019. See note below.
- Zimbabwe has one of the highest maternal mortality ratios in the world, estimated at 651 maternal deaths per 100,000 live births. In contrast to a worldwide trend of declines, maternal mortality has increased in Zimbabwe over the past 25 years.
- Abortion is legally permitted in the country only under limited circumstances, including if the pregnant woman’s life is in danger or in cases of rape, incest or fetal impairment. In practice, it is extremely difficult to obtain a legal abortion; as a result, most abortions are clandestine and potentially unsafe.
- The Zimbabwe Ministry of Health and Child Care has made efforts to increase access to and improve postabortion care in order to reduce maternal mortality. However, ongoing economic insecurity has limited the health system’s capacity to provide these services.
Incidence of abortion
- In 2016, an estimated 65,300 induced abortions occurred in Zimbabwe. This translates to a rate of 17 abortions for every 1,000 women aged 15–49.
- Zimbabwe has one of the lowest abortion rates in Sub-Saharan Africa. In Eastern Africa, which includes Zimbabwe, the regional abortion rate is nearly double, at 34 per 1,000 women aged 15–44.
- Abortion rates in Zimbabwe vary greatly across the country. The highest rates are in the Mashonaland provinces and Harare (21 per 1,000 women aged 15–49) and lowest in the Manicaland and Masvingo provinces (12 per 1,000 women).
Provision of postabortion care
- Of the estimated 25,200 women receiving facility-based postabortion care in 2016, about half were treated for complications related to abortions (many of which were unsafe), and half were treated for complications related to late miscarriage.
- The vast majority (85%) of postabortion care was provided in public health facilities. Half of these cases were treated at district hospitals and one-third at larger, central hospitals.
- Among women treated for postabortion complications in 2016, 78% had mild or moderate complications and 19% had severe complications. Three percent died or nearly died from complications.
Delays and gaps in service provision
- Many women experiencing complications from unsafe abortion or miscarriage in 2016 faced delays in obtaining postabortion care. On average, nearly two full days elapsed between experiencing complications and receiving completed treatment. Common reasons for treatment delays included lack of money, lack of transportation and distance to a health facility.
- Postabortion care is not offered at the majority of primary health centers, which are the facilities most accessible to rural women. Overall, nearly half of postabortion care patients in 2016 had to seek care at more than one facility to get complete treatment.
- One-fifth of public facilities asked women to pay for postabortion care prior to treatment—which caused delays in treatment—even though these facilities are supposed to provide the service at no cost.
- A substantial proportion of first-trimester postabortion cases were treated using surgical procedures not recommended by the World Health Organization (WHO) or national guidelines for this type of care. These procedures are more expensive and carry greater risk for further complications than medically recommended methods such as manual vacuum aspiration and misoprostol (a type of medication).
- More than half of health facilities reported shortages of misoprostol—an essential medicine for postabortion care—in the three months preceding the survey. Half of facilities designated under national guidelines to provide manual vacuum aspiration did not have the equipment to do so. Many other facilities had equipment but were not using it.
- Forty percent of women who had an abortion in Zimbabwe experienced complications that required medical treatment. However, only half of women with complications received the treatment they needed.
Contraception and unintended pregnancy
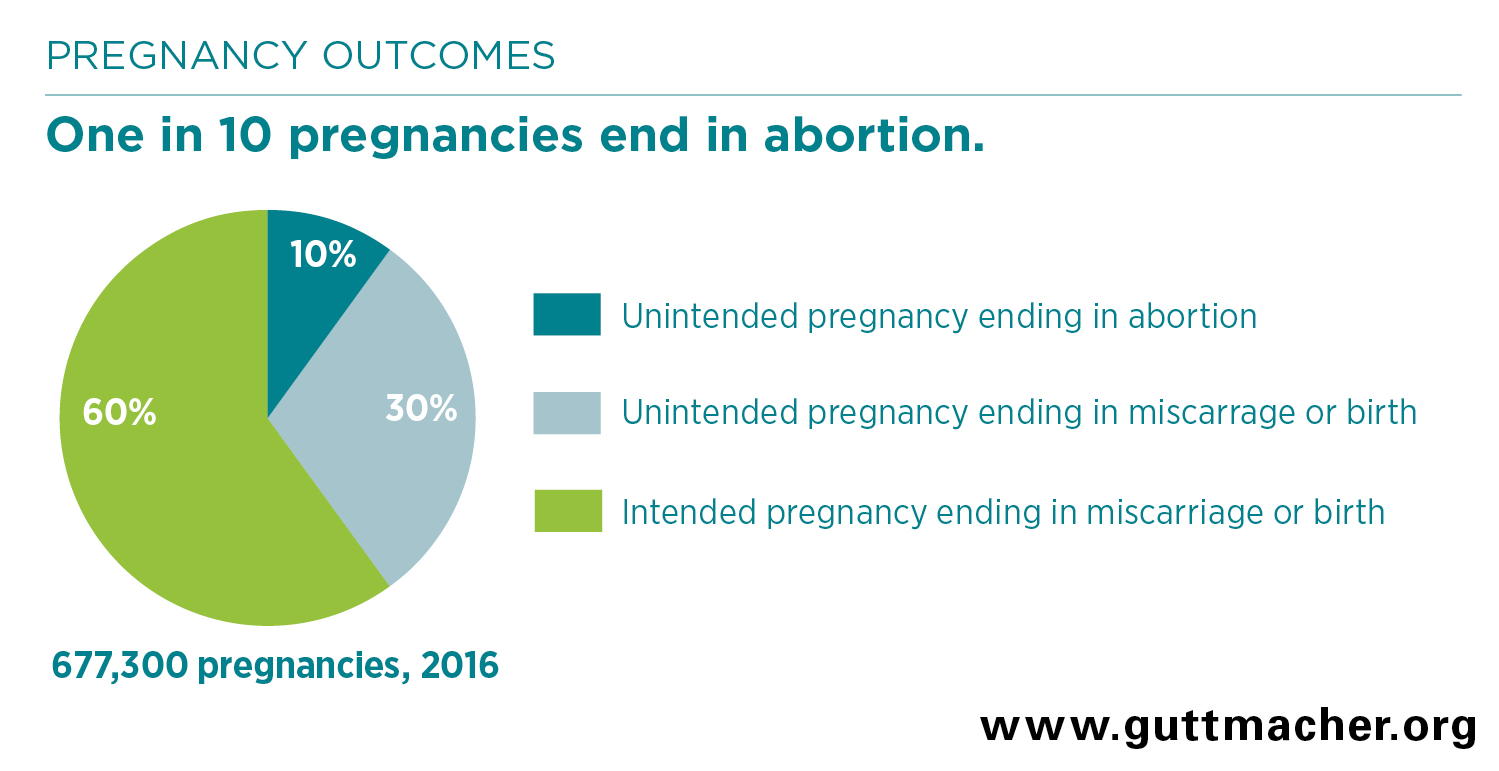
- Most women who have an abortion do so because they become pregnant when they do not intend to. In 2016, 40% of pregnancies in Zimbabwe were unintended and one-quarter of unintended pregnancies ended in abortion.
- Zimbabwe has the highest rate of modern contraceptive use in Sub-Saharan Africa, likely due to the government’s robust family planning program. Two-thirds (66%) of married women and sexually active unmarried women in Zimbabwe used a modern contraceptive method in 2015. Nevertheless, one in 10 married women and two in 10 sexually active unmarried women reported wanting to avoid a pregnancy but were not using any contraceptive method.
Recommendations
- Broaden the circumstances under which abortion is legally permitted, and educate health care professionals and the public about legal provision in order to reduce the number of clandestine and unsafe procedures.
- Ensure the availability of safe, legal abortion services and postabortion care in order to reduce ill health and death from unsafe abortion. Unsafe abortion can result in severe complications, as well as high social and economic costs to women, their families and the health care system. Despite the low national abortion rate, complications from unsafe abortion in Zimbabwe, along with critical gaps in the provision of postabortion care and disparities in access to treatment, contribute to maternal injury and likely to death.
- Increase the availability and use of WHO-recommended postabortion care methods by ensuring facilities have adequate training, supplies and equipment. Specifically, primary health centers should be stocked with adequate supplies of misoprostol. A wide range of providers, including nurses, should be trained and supported to provide both misoprostol and manual vacuum aspiration.
- Increase funding to ensure public health facilities have the resources they need to provide postabortion care free of charge and fully implement the National Guidelines for Com-prehensive Postabortion Care in Zimbabwe.
- Meet women’s and couples’ needs for contraception to help them avoid unintended pregnancies and the unsafe abortions that often follow. Family planning programs should include targeted efforts to reach unmarried young women, poor women and women in rural areas.
NOTE: This fact sheet has been corrected to reflect small changes in the numbers of abortions and pregnancies, which resulted from correcting an error in an underlying data input. These corrections do not change the study’s main findings or conclusions.