As more people choose to postpone pregnancy in response to the ongoing COVID-19 pandemic and economic crisis, some are likely to consider long-acting reversible contraceptives (LARCs).1 These methods, which include IUDs and implants, are both highly effective and low maintenance, making them increasingly popular birth control choices—especially in times of uncertainty about contraceptive coverage and financial prospects.2,3
The LARC renaissance that started in the early 2000s continues to be driven by increased acceptance of contraceptive methods and by policies that encourage LARC availability, affordability and access. Rising LARC use is frequently deemed a public health success that contributes to falling unintended pregnancy and abortion rates (some policymakers—even those who consider themselves abortion rights supporters—view the latter as a societal goal). Reproductive justice advocates and clinical experts recognize that while LARCs are essential for many, they also have a controversial history.4,5 LARCs and programs to promote their use have been—and continue to be—used by the state to control the fertility of Black, Indigenous and other people of color, people with disabilities and people with low incomes.
As more policymakers work to promote LARC access, they must heed the calls of reproductive justice advocates to avoid creating programs that contribute to racist, ableist and coercive contraceptive policies and discourse—or that broadly target marginalized groups rather than prioritize individual needs. To address this issue, SisterSong and the National Women’s Health Network organized reproductive health, rights and justice advocates to create the Long-Acting Reversible Contraception Statement of Principles, which provides a framework—rooted in the experiences of advocates and community members—that warns against potentially coercive and discriminatory rhetoric and policies.6 Together with improved clinical and public health evidence, this framework provides policymakers a map for creating LARC programs that emphasize individual choice and encourage health equity.
Increasing LARC Use and Availability
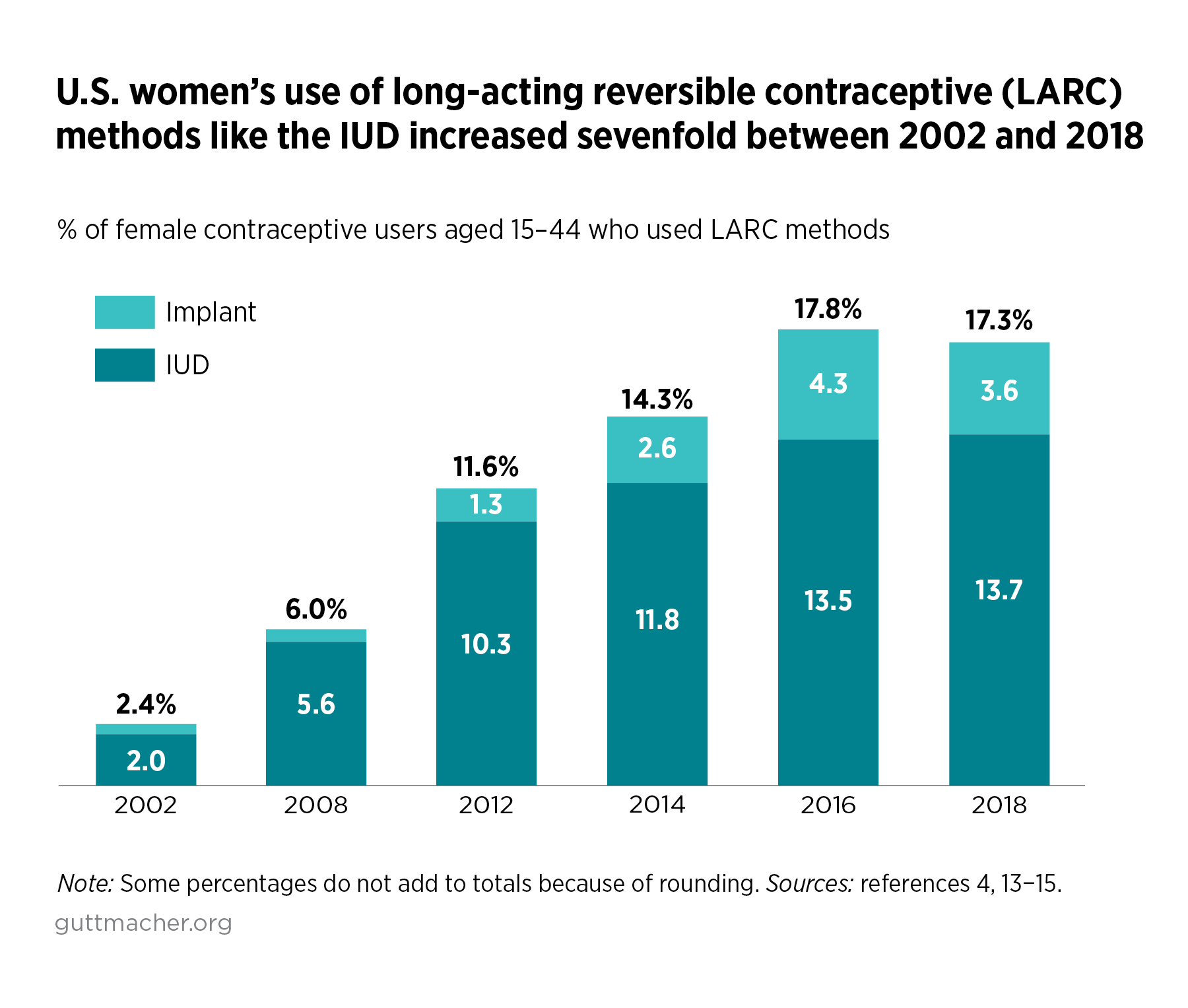
When LARC uptake began increasing in the early 2000s, the methods appeared to be overcoming the bad reputation they earned in the 1970s Dalkon Shield scandal, when that early IUD caused sterilization and other injuries to thousands of women, and by racist, coercive proposals in the 1990s that would have forced people to use the Norplant implant in order to receive welfare and charitable services.7–9 As more options were introduced, LARCs were viewed as exciting "new" methods: Multiple types of hormonal IUDs were introduced, as well as a new implantable device.10,11 Clinical guidance made it clear that, contrary to what many clinicians had believed, LARCs were appropriate for young people and those who had not yet given birth.12 This guidance helped to increase the methods’ popularity: Over the last two decades, LARC use has increased substantially among all contraceptive users (see figure), and LARC use more than doubled among 15–19-year-olds just between 2014 and 2016.4,13–15
This renaissance also coincided with major policy changes that promoted contraceptive access broadly, and, in some states, promoted LARCs specifically. These changes have been given some credit for a significant decline in the U.S. unintended pregnancy rate, particularly among adolescents.16 While LARCs are only one driver of this decrease, some researchers and policymakers laud their role in reducing unintended pregnancy as a public health success story.17,18
Perhaps the policy change that increased LARC access the most has been the Affordable Care Act’s (ACA) contraceptive coverage guarantee, which requires plans to cover all methods without any copayments or other patient out-of-pocket costs.19 While LARCs are incredibly cost effective, lasting for months or even years, they come with a high up-front cost, often upward of $1,000.20,21 Not only did more people get coverage through private insurance or state Medicaid programs under the ACA, they could now choose the contraceptive method that worked best for them without being constrained by cost.
Policymakers in some states have built on this foundation. To mitigate the impact of federal policy changes under the Trump-Pence administration and future hostile administrations, and to provide clarity to consumers and insurers, 16 states have codified the ACA contraceptive coverage guarantee’s ban on cost-sharing.22 Many of these states also codified the federal policy’s requirement to cover related services, including LARC insertion and removal, and to prohibit insurance red tape that leads to restrictions and delays—frequent barriers for people desiring LARCs.
In addition to requiring contraceptive coverage, federal and state policymakers have taken additional steps to make LARCs affordable and accessible to low-income populations. Federal Medicaid guidelines make it clear that state programs must cover LARC removal and reinsertion regardless of reason.23 Further, state Medicaid programs have started unbundling payments for LARC insertion from other postpartum care to eliminate financial disincentives for providers to offer a service deemed critical by maternal health experts.10,24,25 Finally, states have continued to invest in family planning programs to reduce disparities in access. For example, Virginia’s LARC expansion program has reimbursed providers for LARC devices and services for low-income people, most of whom are Black or Hispanic.26,27
Reducing LARC cost is only one part of the access formula. Devices need to be readily available, and providers trained to offer them to patients. The Title X family planning program has enabled more sites, including federally qualified health centers, to keep IUDs and implants in stock by covering the devices’ up-front costs. In turn, this allows patients to have a LARC inserted during the same visit as their consultation.28
Private groups, such as Upstream USA, have also helped public clinics keep LARCs on hand.29 Programs initiated by these groups also offer training for providers, including physicians, advanced practice nurses and physician assistants, to insert and remove LARCs and to provide patient-centered contraceptive counseling. The private-public partnerships offered by Upstream have been credited with helping to reduce the unintended pregnancy rate, particularly among youth, in several states. For example, the unintended pregnancy rate in Delaware dropped 25% over three years after Upstream’s program began.30 Significant state investment in sexual and reproductive health infrastructure, including a training partnership with Upstream, appears to have empowered people in Delaware to choose if and when to become pregnant—the most desirable outcome for contraceptive programs.31
A History of Coercion and Guarding Against It
Since LARCs were introduced, they have been used as part of discriminatory campaigns targeting Black, Indigenous and other people of color, disabled people and people with low incomes. Programs that tied benefits to LARC use and that targeted marginalized communities made explicit the racist, ableist and classist beliefs of policymakers.32 This history and years of advocacy by reproductive justice activists in response serve as warnings to policymakers and clinicians considering interventions.
From the above-mentioned Dalkon Shield scandal through the 2000s, LARCs have been associated with reproductive harm and coercion, particularly against young Black and Latina people.9 For example, almost immediately after Norplant was introduced in the early 1990s, pundits and policymakers proposed that its use be incentivized, or even mandated, for people receiving welfare benefits. While no legislature passed such a mandate, other financial incentive programs still heavily pushed Norplant for teens and low-income people.33 Many Norplant recipients found that their providers refused to remove the device and that Medicaid would not cover removal, even as they experienced unbearable side effects or desired to get pregnant.34 These programs and policies carried a significant message: Low-income individuals, especially Black, Indigenous or other people of color, should not be having children. This message was yet another example of the racism long endemic to the United States.
While advocacy and practice have shifted the LARC conversation among policymakers to be more justice-oriented, the legacy of reproductive coercion continues into the 21st century. Some states continue to have so-called family caps on public assistance, which deny additional aid for families that have more children as a way to coerce people into having smaller families than they might want.35 As recently as 2017, judges offered reduced sentencing to people if they received an IUD or were sterilized, and in 2020, reports emerged of forced sterilization in immigrant detention facilities.36,37
Similarly, the public health and advocacy discourse often echoes the same negative messages: Some researchers and policymakers portray the prevention of unintended pregnancy as key to breaking the poverty cycle and reducing taxpayer burdens—a view that perpetuates stigma against young parents and low-income people.17 Other experts have countered this view by showing how painting LARCs as "a powerful new tool to fight poverty" is reminiscent of more than a century of eugenicist thought and promotion of reproductive control.17,38,39 These experts warn that policymakers may unintentionally fall into the same discriminatory and stigmatizing rhetorical traps by singling out specific populations for LARC promotion.
Take, for example, programs that target people who use illegal substances. Policymakers may wish to offer LARC services in areas that have high rates of opioid use, thinking that the program will help reduce unintended pregnancy and, through that, neonatal abstinence syndrome, a condition that can affect newborns of substance users and lead to long-term health problems.40 However, in environments such as harm reduction clinics and correctional facilities, people may feel pressured into making a contraceptive choice as a result of unequal power dynamics. Particularly in these programs, people should be offered a full range of contraceptive options and, ideally, be provided additional, targeted support. For example, West Virginia’s family planning program trains providers how to counsel people with substance use disorders and offers additional funding for LARC promotion to help ensure access to counseling and these higher-cost methods at more sites.41,42 Without safeguards such as noncoercive counseling, these types of programs can unintentionally send the message that some people—people who use illegal substances, are incarcerated or are otherwise considered "unfit" to parent—should use LARCs.
Providers, too, introduce bias and perpetuate stigma when treating and counseling patients. The structural racism, sexism and ableism that pervade society also influence medical providers, who may be more likely to push LARCs to Black, Indigenous or other patients of color or to patients who are low income or disabled.43 An emphasis on efficacy in guidance from major professional organizations, including the World Health Organization, American College of Obstetricians and Gynecologists (ACOG) and American Academy of Pediatrics (AAP), can also unintentionally encourage overly directive counseling for these patient groups.44–46 While many providers already temper their enthusiasm for LARCs, the opportunity for bias remains without clear and culturally competent guidelines and training for providers at all levels of care. Provider bias, in turn, often results in mutual distrust with patients, producing a cycle that reduces quality of care.47
Looking Ahead on LARC Access
LARCs are an evidence-based, popular category of contraception, and it is clear that state and private programs to expand access can be effective. At the same time, policymakers and clinicians must heed the lessons of past and current programs and advocacy to create policies that are consistent with reproductive justice values.
Utilizing a person-centered framework. Contraceptive programs should be based on a person-centered framework that ensures equitable access and patient well-being.48 These frameworks use individualized counseling to serve and empower patients; provide support to marginalized communities without further stigmatizing them; and offer services that are accessible to the local population and staffed by a range of providers who reflect the community itself. For example, Upstream USA has implemented the SisterSong and National Women’s Health Network’s principles to help providers avoid the trap of "one-size-fits-all" contraceptive counseling.49 These guidelines, similar to those established for the Title X national family planning program, recognize that people have a variety of contraceptive needs and desires and help providers better serve those needs. Programs should also prioritize reducing barriers to care by providing same-day access to LARC insertion—including as part of postpartum services—and removal, without delays or additional costs.
Giving patients options with nondirective counseling. The enthusiasm for LARCs stems from a clinical emphasis on efficacy, but providers and advocates know that patients need to be given a full range of options.50 Professional organizations such as the AAP are updating their guidance to explicitly caution against unintentionally directive counseling that results from the "overwhelmingly favorable" attention LARCs get from public health experts.51 In a 2020 commentary, obstetrician-gynecologist Kristyn Brandi and Guttmacher researcher Liza Fuentes provide guidance in avoiding the pitfalls of a tiered-efficacy approach (one that prioritizes methods with higher efficacy over others) and mitigating the potential for coercion through nondirective counseling.52 For example, providers may use tools like "One Key Question," which asks patients, "Would you like to become pregnant in the next year?" to open fuller, patient-directed conversations about reproductive goals, or the popular Reproductive Health Access Project (RHAP) "Your Birth Control Choices" fact sheet, which has recently been updated to present contraceptive options in an order that seems least likely to bias choice—alphabetically.53,54
Avoiding incentives—intended or not—for LARCs. Programs must be carefully structured so as not to create what Brandi and Fuentes call a "nonchoice," in which highly effective methods like LARCs are offered at no cost but other methods incur a fee. ACOG warns in an official statement that a policy inappropriately incentivizing the start or discontinuation of specific methods, whether financially or as a condition of aid or sentencing, "directly compromises individual agency and autonomy" and is thus coercive.55 Rather, policymakers should promote coverage of and access to comprehensive contraceptive care—including the full range of methods and services, same-day insertion and removal of LARC methods, and postpartum LARC placement—to ensure that people can make contraceptive choices without feeling pressured by cost concerns or political developments, such as changing administrations, courts or policies.56
Fostering trust by reducing racial bias. Patients need to be able to trust their providers, especially for intimate services like contraception. However, people of color report feeling distrusted and having their concerns dismissed by their providers.33 The resulting cycle of distrust reduces quality of care, with consequences that go beyond contraceptive provision to people’s overall health. Providers and their support staff need substantial and ongoing training on antiracism, bias and cultural humility to better serve their patients. Further, research shows that patients of color receive better care when their provider is also a person of color—making diversity in medicine an imperative.57
Following the lead of the community. Reproductive justice advocates point to intergenerational conversations and change as inflection points for contraceptive access. Varied experiences of contraception and parenting, as well as the United States’ long history of reproductive oppression, influence contrasting generational attitudes toward LARCs. Community engagement in these conversations is essential to programs that address misconceptions and inequities with nuance. For example, in New Mexico, the reproductive justice organization Bold Futures led a coalition in creating a statewide program that incorporates cultural competency and noncoercive counseling training to better serve its population.58,59
As policymakers consider programs to expand LARC access, they must be aware of these examples and adhere to these principles. Programs must not only be effective in reducing costs, expanding availability and training providers. They must protect people against coercion and bias and empower individuals to choose contraceptive methods that suit their needs.