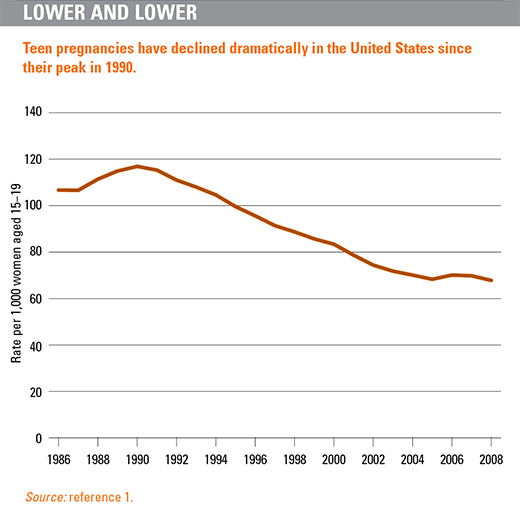
Adolescent pregnancies have declined dramatically in the United States since their peak in the early 1990s, and in 2008, the pregnancy rate reached its lowest level in nearly 40 years. That year, the pregnancy rate was 68 per 1,000 women aged 15–19, representing a 42% decline since 1990 (see chart).1 The long-term decline in teen pregnancy appears to have been driven primarily by improved use of contraception. In other words, adolescents seem to be practicing contraception more effectively, and their actions are paying off in lower pregnancy rates, and lower birth and abortion rates, as well.
Even with these encouraging trends, however, adolescent pregnancy remains a serious public health concern. Each year, nearly 750,000 U.S. women aged 15–19 become pregnant,1 an overwhelming majority (82%) report that their pregnancy was unplanned.2 Moreover, the United States still has substantially higher levels of adolescent pregnancy, childbearing and abortion than other industrialized countries: A 2013 report from the National Research Council and the Institute of Medicine compared the United States with 16 peer countries—affluent democracies that include Australia, Canada, Japan and many western European countries—and found that the United States had the highest teen birthrate.3
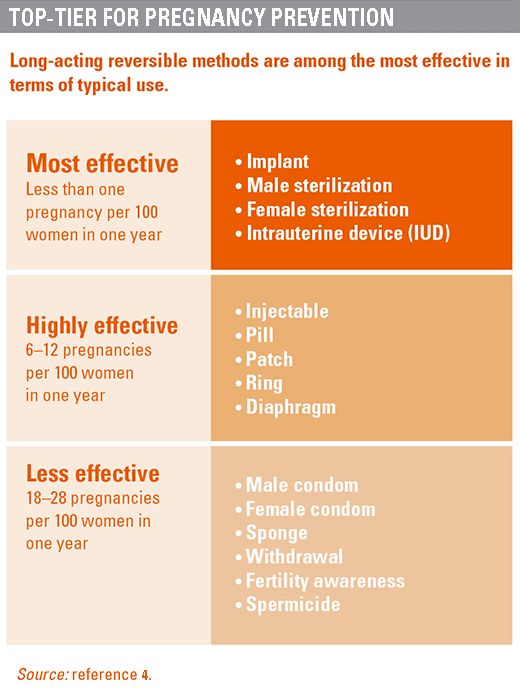
Reproductive health professionals, therefore, are looking at ways to help more U.S. teens to avoid unintended pregnancy, and one approach is increased access to long-acting reversible contraceptive (LARC) methods—namely, copper and hormonal intrauterine devices (IUDs) and hormonal implants. With failure rates of less than 1%, LARCs are the most effective methods of reversible contraception on the market today.4 And yet, most adolescents and young women have never heard of an IUD or implant, many health care providers remain misinformed about their risks, and numerous practical obstacles stand in the way of more fully integrating LARCs into the range of contraceptive methods offered to adolescents and young women.
Taking Responsibility
A few key factors have driven the long-term declines in teen pregnancy, birth and abortion rates. Teens are waiting longer to have sex: The likelihood of sexual activity among adolescents (at any given age) is lower now than at any time in the past 25 years.5 At the same time, a large body of research shows that today’s teens are far better contraceptive users than prior generations of teens. It is now the norm for teens to use contraceptives at first sex, which creates a pattern of continued contraceptive use down the road.6 Among females aged 15–19, contraceptive use at first sex increased steadily, from 48% in 19827 to 78% in 2006–2010;8 contraceptive use at last sex among adolescent women also improved, particularly in recent years, from 71% in 1995 to 86% in 2006–2010.
Moreover, adolescents increasingly use more effective methods and use a condom with another method for dual protection against pregnancy and STIs. Among never-married sexually active women aged 15–19, 43% reported in 2006–2010 using hormonal methods—mostly the pill, but also the injectable, patch or ring—at last sex in the prior three months, and 20% reported dual use of both the condom and a hormonal method.8
Although contraceptive use is now the norm, there is still room for improvement. When used perfectly, condoms and the pill have extremely low failure rates.4 But in the real world, many couples have difficultly using these methods consistently and correctly—every day for the pill or at every act of intercourse for the condom—and, therefore, experience a higher risk of failure. Teens are especially likely to experience a contraceptive failure: Adolescent women are more than twice as likely as women aged 30 or older to experience a pill failure, for example.9
Rethinking LARCs
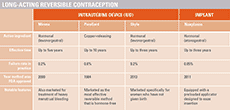
LARCs are easy to use and extremely effective once in place. Four LARC products are available in the United States today—a copper IUD, two hormonal IUDs and a hormonal implant—and they all provide long-term, but not permanent, pregnancy protection (see table).
For adolescents, LARCs offer several advantages over other contraceptive methods. Because there is virtually no possibility of user error, IUDs and implants rank in the top tier of contraceptive methods in terms of effectiveness (see chart).4 The "set and forget" nature of LARCs may be appealing to teens who do not want to worry about remembering to use a contraceptive. Plus, once the IUD or implant is in place, it prevents pregnancy for years—during a time when most teens want to avoid childbearing. On average, young people have sex for the first time at about age 17, but do not marry or have a child until their mid-20s.10 As a result, adolescents and young adults typically spend nearly a decade trying to avoid pregnancy.
According to the U.S. practice recommendations for contraceptive use, released by the Centers for Disease Control and Prevention (CDC) in 2013, LARCs are appropriate for adolescents.11 The report, based on global guidance from the World Health Organization, emphasizes that contraceptive method effectiveness is a "critically important" element when choosing a method, and LARCs are "highly effective because they do not depend on regular compliance from the user."
Similarly, the American College of Obstetricians and Gynecologists (ACOG) describes LARCs as "first-line" options for all women and adolescents on the basis of their "top-tier effectiveness, high rates of satisfaction and continuation, and no need for daily adherence."12 The opinion, released in 2012, is a reaffirmation of one issued in 2007, and it examines the key evidence and benefits of adolescent LARC use. It concludes that counseling about LARCs should occur at all health care provider visits with sexually active adolescents, and that adolescents who use LARCs should also be advised to consistently use condoms for the prevention of STIs.
Obstacles: Real and Perceived
Armed with these practice guidelines, health care providers and advocates are working to overcome a number of obstacles to teens’ access to LARCs. All of these obstacles are surmountable, and some progress has already been made through better education and training, and by making LARCs more affordable.
Infection. IUDs had not traditionally been recommended for adolescents because they had been perceived to be at an elevated risk of infection. Indeed, the Dalkon Shield—an IUD introduced to the U.S. market in the early 1970s—was plagued by a cluster of serious and even fatal health risks, including pelvic inflammatory disease (PID) and subsequent infertility. Today, the Dalkon Shield is widely acknowledged to have had a flawed design; the copper and hormonal IUDs on the market today are considered safe on all counts.
This is not to say that adolescents’ risk of infection—and of subsequently developing PID—can be ignored. Because adolescents often have multiple partners and their STI rates are high, the CDC and ACOG both recommend that health care providers screen adolescents for STIs and counsel them on the importance of condom use along with LARCs.11,12 Strong evidence suggests, however, that the risk of PID and infertility is greatly reduced if a woman is tested and, if necessary, treated for STIs when or before an IUD is inserted.12 Any issues with infection are likely caused by the insertion process, not the IUD itself.
Despite evidence to the contrary, however, some medical providers still associate the IUD with infection risks and liability concerns, and are reluctant to offer the method to their younger patients.13,14 In addition, some providers are concerned that they would lose opportunities to provide their young patients who chose LARCs with other health services, such as STI screenings, because such adolescents might not return to the clinic for the duration of the method’s coverage.15 ACOG and other medical groups are working to overcome these and other provider concerns, and to address common misconceptions. Product manufacturers have also developed educational programs and training kits focused on the appropriate use of IUDs and proper steps for insertion to avoid infections.16
Insertion, fit and expulsion. Concerns about the fit of the IUD in young patients have also contributed to clinicians’ reluctance to offer the method to adolescents. According to the ACOG opinion, little evidence suggests that IUD insertion is technically more difficult in adolescents than in older women.12 However, young women are at a slightly increased risk of IUD expulsion if they have never given birth, and more than half report discomfort with insertion. To address these concerns, ACOG recommends improvements in residency training and continuing medical education, not only in insertions but also to review the key evidence and benefits of adolescent LARC use.
A new IUD, sold under the trade name Skyla, may help assuage concerns of adolescents and providers. Skyla is slightly smaller than the other IUDs available on the market today and was specifically designed for women who have not had a child. The device is the first new IUD to be brought to the U.S. market in 13 years.
Adolescents’ concerns. According to a Guttmacher study on LARCs that included 48 in-depth interviews with women aged 16–24, adolescents and young women questioned whether the IUD or implant was an appropriate method choice for them.15 They expressed concern about having a foreign object in their body, negative side effects and pain associated with insertion and removal. Moreover, although the long-acting nature of LARCs was seen as a positive feature by some women, others saw the duration of 3–10 years as too long for them to consider.
These concerns are legitimate: Adolescents who use an IUD or implant can expect some pain and side effects, including changes in their bleeding patterns.12 Health care providers should counsel adolescents to expect such side effects, advise them on how to manage any pain or bleeding experienced, and reassure them that their device can be removed at any time. As a matter of fact, providers should address these types of issues when counseling adolescents on the full range of contraceptive options and help them understand the differences among methods, so they can choose one that is best for them.
Cost. For a woman who does not plan to have a child in the next few years, IUDs and implants are highly cost-effective: After the initial cost of the device and its insertion, LARCs require only occasional check-ins and, eventually, removal. Yet, that up-front cost could be a significant hurdle. For clinics, the wholesale cost of an IUD or implant can be as high as $850, plus the cost of insertion.17
The good news is that financial barriers to LARCs already are starting to fall, thanks to the Affordable Care Act (ACA). Several provisions in the ACA should improve coverage for contraceptive services, including LARCs. First, by expanding eligibility for Medicaid and providing federal subsidies to purchase private insurance on new health insurance marketplaces, the ACA is extending comprehensive health coverage—including coverage for contraceptive methods and counseling—to millions of women who would otherwise be uninsured. Moreover, the ACA includes a requirement that insurance plans allow individuals to remain on their parents’ policy through age 26, which should mean better LARC coverage for young women. And finally, most women’s insurance—whether Medicaid or private coverage—now covers contraception without out-of-pocket costs (related article). For most plans, that should include LARC devices and all related services, including counseling, STI testing, insertion, follow-up care and removal.
Real Contraceptive Choice
Research indicates that when financial barriers are completely removed and counseling is provided on all methods, women choose LARCs in large numbers. The Contraceptive CHOICE Project in St. Louis is a longitudinal, observational study of women’s choice, use and continuation of reversible contraceptive methods.18 Between 2007 and 2009, the study enrolled about 5,000 women aged 14–45, including 1,000 aged 14–20. All participants were offered the full range of reversible contraceptive methods at no cost for three years, and 62% of 14–20-year-olds and 70% of women overall chose a LARC method over a short-acting method. An analysis of data from the Contraceptive CHOICE Project found that most adolescents who opt for LARCs continue to use them: Two years after choosing a method, 67% of adolescents who selected a LARC were still using their method, compared with 37% of youth who selected another method type.19
Even in the absence of these ideal, experimental conditions, LARCs have become increasingly popular nationwide. The proportion of U.S. female contraceptive users currently using an IUD or implant rose substantially between 2002 and 2009, from 2.4% to 8.5%.20 Even among women aged 15–19, LARC use increased over the period, from less than 1% to 4.5%—a trend driven almost entirely by increased use among older teens.
Still, LARC use remains relatively low, and many adolescents and young women report they know little or nothing about the methods. One nationally representative study, commissioned by the National Campaign to Prevent Teen and Unplanned Pregnancy, and conducted by the Guttmacher Institute, gathered detailed results from a sample of 1,800 unmarried men and women aged 18–29.21 It found that 69% of young adults aged 18–19 had heard of the IUD, and just 38% said they had ever heard of the implant. Another survey of 252 women aged 14–27 presenting for care at a clinic in California in 2007 found that fewer than half of participants (45%) had heard of the IUD.22
This is unfortunate: Young women may welcome information about the IUD and implant when being counseled on contraception. Adolescents—like all women seeking reproductive health services—should be able to pick a contraceptive method that is right for them. In the words of the ACOG opinion on LARCs, "patient choice should be the principal factor in prescribing one method of contraception over another."12 For real contraceptive choice, adolescents need complete and accurate information on all methods and for as many of the practical barriers as possible to be removed. Fewer cost barriers for long-acting methods, increased provider training and greater awareness of these options among adolescents themselves are currently in the works and may well translate to more young women choosing LARCs. That would enable more of them to have greater control over their own reproductive lives—a win for them and for society at large.
REFERENCES
1. Kost K and Henshaw S, U.S. Teenage Pregnancies, Births and Abortions, 2008: National Trends by Race and Ethnicity, New York: Guttmacher Institute, 2012, <http://www.guttmacher.org/pubs/USTPtrends08.pdf>, accessed Nov. 16, 2013.
2. Finer LB and Zolna MR, Unintended pregnancy in the United States: incidence and disparities, 2006, Contraception, 2011, 84(5):478–485.
3. Woolf SH and Aron L, eds., U.S. Health in International Perspective: Shorter Lives, Poorer Health, Washington, DC: The National Academics Press, 2013.
4. Hatcher RA et al., Contraceptive Technology, 20th ed. New York: Ardent Media, 2011.
5. Finer LB and Philbin JM, Sexual initiation, contraceptive use, and pregnancy among young adolescents, Pediatrics, 2013, 131(5):886–891.
6. Shafii T et al., Is condom use habit forming?: condom use at sexual debut and subsequent condom use, Sexually Transmitted Diseases, 2004, 31(6):366–372.
7. Mosher WD and Bachrach CA, Contraceptive use, United States, 1982, Vital and Health Statistics, 1986, Series 23, No. 12, <http://www.cdc.gov/nchs/data/series/sr_23/sr23_012.pdf>, accessed Nov. 17, 2013.
8. Martinez G et al., Teenagers in the United States: sexual activity, contraceptive use, and childbearing, 2006–2010 National Survey of Family Growth, Vital and Health Statistics, 2011, Series 23, No. 31, <http://www.cdc.gov/nchs/data/series/sr_23/sr23_031.pdf>, accessed Nov. 17, 2013.
9. Kost K et al., Estimates of contraceptive failure from the 2002 National Survey of Family Growth, Contraception, 2008, 77(1):10–21.
10. Gold RB et al., Next Steps for America’s Family Planning Program: Leveraging the Potential of Medicaid and Title X in an Evolving Health Care System, New York: Guttmacher Institute, 2009, <http://www.guttmacher.org/pubs/NextSteps.pdf>, accessed Nov. 17, 2013.
11. Centers for Disease Control and Prevention, U.S. selected practice recommendations for contraceptive use, 2013, Morbidity and Mortality Weekly Report, 2013, 62(5):1–60, <http://www.cdc.gov/mmwr/pdf/rr/rr62e0614.pdf>, accessed Nov. 17, 2013.
12. American College of Obstetricians and Gynecologists, Committee on Adolescent Health Care, Long-Acting Reversible Contraception Working Group, Committee opinion no. 539: adolescents and long-acting reversible contraception: implants and intrauterine devices, Obstetrics & Gynecology, 2012, 120(4):983–988.
13. Madden T et al., Intrauterine contraception in Saint Louis: a survey of obstetrician and gynecologists’ knowledge and attitudes, Contraception, 2010, 81(2):112–116.
14. Kavanaugh ML et al., Meeting the contraceptive needs of teens and young adults: youth-friendly and long-acting reversible contraceptive services in U.S. family planning facilities, Journal of Adolescent Health, 2012, 52(3):284–292.
15. Kavanaugh ML et al., Long-acting reversible contraception for adolescents and young adults: patient and provider perspectives, Journal of Pediatric and Adolescent Gynecology, 2013, 26(2):86–95.
16. Piazza C, Bayer HealthCare, Whippany, NJ, personal communication, Oct. 25, 2013.
17. Trussell J, Update on and correction to the cost-effectiveness of contraceptives in the United States, Contraception, 2012, 85(2):218.
18. Mestad R et al., Acceptance of long-acting reversible contraceptive methods by adolescent participants in the Contraceptive CHOICE Project, Contraception, 2011, 84(5):493–498.
19. O’Neil-Callahan M et al., Twenty-four-month continuation of reversible contraception, Obstetrics & Gynecology, 2013, 122(5):1083–1091.
20. Finer LB, Jerman J and Kavanaugh ML, Changes in use of long-acting contraceptive methods in the United States, 2007–2009, Fertility and Sterility, 2012, 98(4):893-897.
21. Kaye K, Suellentrop K and Sloup C, The Fog Zone: How Misperceptions, Magical Thinking, and Ambivalence Put Young Adults at Risk for Unplanned Pregnancy, Washington, DC: The National Campaign to Prevent Teen and Unplanned Pregnancy, 2009, <http://www.thenationalcampaign.org/fogzone/PDF/FogZone.pdf>, accessed Nov. 17, 2013.
22. Fleming KL, Sokoloff A and Raine TR, Attitudes and beliefs about the intrauterine device among teenagers and young women, Contraception, 2010, 82(2):178–182.